Key Points
The updated Vienna Prediction Model was developed to identify patients with unprovoked VTE who are at low risk of recurrence.
In elderly patients with unprovoked VTE, the model does not discriminate between patients who develop recurrent VTE and those who do not.
Abstract
The updated Vienna Prediction Model for estimating recurrence risk after an unprovoked venous thromboembolism (VTE) has been developed to identify individuals at low risk for VTE recurrence in whom anticoagulation (AC) therapy may be stopped after 3 months. We externally validated the accuracy of the model to predict recurrent VTE in a prospective multicenter cohort of 156 patients aged ≥65 years with acute symptomatic unprovoked VTE who had received 3 to 12 months of AC. Patients with a predicted 12-month risk within the lowest quartile based on the updated Vienna Prediction Model were classified as low risk. The risk of recurrent VTE did not differ between low- vs higher-risk patients at 12 months (13% vs 10%; P = .77) and 24 months (15% vs 17%; P = 1.0). The area under the receiver operating characteristic curve for predicting VTE recurrence was 0.39 (95% confidence interval [CI], 0.25-0.52) at 12 months and 0.43 (95% CI, 0.31-0.54) at 24 months. In conclusion, in elderly patients with unprovoked VTE who have stopped AC, the updated Vienna Prediction Model does not discriminate between patients who develop recurrent VTE and those who do not. This study was registered at www.clinicaltrials.gov as #NCT00973596.
Introduction
Unprovoked venous thromboembolism (VTE) is associated with a 5% to 27% annual risk of recurrence after discontinuation of anticoagulation (AC),1-4 and indefinite AC is recommended if the bleeding risk is low to moderate.5 However, in one-third of patients with unprovoked VTE, the risk of recurrence is so low (<3% per year) that anticoagulant therapy >3 months may not be necessary.4,6 Several prediction rules were derived to identify patients with unprovoked VTE who have a low recurrence risk.4,7-9 One is the original Vienna Prediction Model, which was derived in 929 patients (median age, 54 years) with a first unprovoked VTE.8 Based on 3 parameters, sex, location of VTE (pulmonary embolism [PE]/proximal deep vein thrombosis [DVT] vs distal DVT), and a quantitative D-dimer level determined by enzyme-linked immunosorbent assay (ELISA) at 3 weeks after discontinuation of AC, the risk of recurrent VTE can be estimated. In an external validation study enrolling 904 older patients (median age, 68 years), the model showed a less than optimal calibration, underestimating the observed cumulative recurrence rates at 12 months.10
The updated Vienna Prediction Model is an improved version of the original Vienna Prediction Model and allows prediction of recurrence at several different time points after stopping AC.9 It was developed in a prospective cohort of 553 patients with unprovoked VTE and uses the same clinical parameters (ie, sex, location of VTE, and a quantitative D-dimer level determined by ELISA between 3 weeks and 15 months after discontinuation of AC) to estimate the risk of recurrent VTE up to 60 months, using nomograms or a web-based calculator (www.meduniwien.ac.at/user/georg.heinze/dvpm/).9 To our knowledge, the updated Vienna Prediction Model has never been externally validated. We aimed to validate the accuracy of the updated Vienna Prediction Model to predict recurrence in elderly patients with unprovoked VTE. Given that elderly patients are at higher risk of bleeding,11 it is important to avoid extended AC in elderly patients who have a low recurrence risk.
Study design
This study was performed as part of a prospective multicenter cohort to assess medical outcomes in elderly patients with acute, symptomatic VTE from 9 Swiss university and non-university hospitals between September 2009 and December 2013.12 A detailed description of the study methods has been published previously.12 Briefly, consenting consecutive patients aged ≥65 years with objectively diagnosed, symptomatic DVT or PE were prospectively identified and followed over time. The ethics committee at each participating center approved the study, which followed the Helsinki protocol. For the sake of this analysis, only patients with unprovoked VTE (defined as VTE in the absence of immobilization, major surgery, oral estrogen therapy, or active cancer during the last 3 months) and who had completed a 3- to 12-month course of AC were included.
Patients underwent quantitative D-dimer testing (ELISA, VIDAS, bioMérieux) at 12 months after the index VTE. Only patients who were off anticoagulants at the time of D-dimer measurement were included. Follow-up started after D-dimer measurement, ie, 12 months after the index VTE. The outcome was the recurrence of symptomatic, objectively confirmed VTE within 12 and 24 months of D-dimer testing, defined as symptomatic new DVT or PE, based on predefined imaging criteria or autopsy as previously described.12 Three blinded, independent experts adjudicated all recurrences.
We determined the proportion of patients classified as low-risk (lowest quartile of predicted 12-month risk of VTE recurrence) according to the updated Vienna Prediction Model and compared the proportion of VTE recurrence at 12 and 24 months between low- and higher-risk patients. We examined the goodness-of-fit of the model at 12 and 24 months using the Hosmer–Lemeshow test. We also assessed the discriminative power of the model by calculating the area under the receiver operating characteristic (ROC) curve for VTE recurrence at 12 and 24 months. Our primary analysis included all patients with unprovoked VTE. In a subgroup analysis, we excluded all patients who had a prior VTE before the index event. Analyses were done using Stata 13 (Stata Corporation, College Station, TX).
Results and discussion
Overall, 1003 patients were initially enrolled in our cohort. After the exclusion of 394 patients with cancer-related or provoked VTE (14 had hormone therapy), 280 who received anticoagulants beyond 12 months, 167 without D-dimer measurement, and 6 without initial AC therapy, our final study sample comprised of 156 patients with acute unprovoked VTE. A total of 20 patients with unprovoked VTE were excluded because they had recurrent VTE between AC discontinuation and start of follow-up, and thus were still under anticoagulants (n = 12) or had no D-dimer measurement (n = 8). Of these, 40% were men and 90% had PE/proximal DVT. Overall, there was no age and sex difference between excluded and analyzed patients (data not shown).
Analyzed patients had a median age of 74 years, 41% were women, and 88% had PE or proximal DVT as the initial VTE event (Table 1). Low-risk patients were less likely to be men and to have PE/proximal DVT, and had lower D-dimer levels than higher-risk patients.
Patient baseline characteristics
| . | All (N = 156) . | Low-risk patients (N = 39) . | Higher-risk patients (N = 117) . | P . |
|---|---|---|---|---|
| . | n (%) or median (interquartile range) . | . | ||
| Age (y)* | 74.0 (69.0; 79.8) | 73.0 (68.0; 77.0) | 75.0 (69.0; 80.0) | .27 |
| Male sex | 92 (59) | 4 (10) | 88 (75) | <.01 |
| PE and/or proximal DVT | 137 (88) | 28 (72) | 109 (93) | <.01 |
| D-dimer (ng/ml)† | 1022 (607; 1755) | 717 (410; 1016) | 1161 (694; 1913) | <.01 |
| BMI (kg/m2)* | 27.5 (24.8; 30.5) | 27.7 (24.9; 31.9) | 27.5 (24.8; 30.4) | .44 |
| Prior VTE | 23 (15) | 8 (21) | 15 (13) | .30 |
| Time since stopping AC (mo)† | 5.7 (4.9; 6.9) | 5.9 (5.0; 7.6) | 5.6 (4.7; 6.6) | .20 |
| Duration of prior AC (mo) | 6.3 (5.3; 7.1) | 6.0 (4.1; 6.9) | 6.4 (5.5; 7.2) | .20 |
| . | All (N = 156) . | Low-risk patients (N = 39) . | Higher-risk patients (N = 117) . | P . |
|---|---|---|---|---|
| . | n (%) or median (interquartile range) . | . | ||
| Age (y)* | 74.0 (69.0; 79.8) | 73.0 (68.0; 77.0) | 75.0 (69.0; 80.0) | .27 |
| Male sex | 92 (59) | 4 (10) | 88 (75) | <.01 |
| PE and/or proximal DVT | 137 (88) | 28 (72) | 109 (93) | <.01 |
| D-dimer (ng/ml)† | 1022 (607; 1755) | 717 (410; 1016) | 1161 (694; 1913) | <.01 |
| BMI (kg/m2)* | 27.5 (24.8; 30.5) | 27.7 (24.9; 31.9) | 27.5 (24.8; 30.4) | .44 |
| Prior VTE | 23 (15) | 8 (21) | 15 (13) | .30 |
| Time since stopping AC (mo)† | 5.7 (4.9; 6.9) | 5.9 (5.0; 7.6) | 5.6 (4.7; 6.6) | .20 |
| Duration of prior AC (mo) | 6.3 (5.3; 7.1) | 6.0 (4.1; 6.9) | 6.4 (5.5; 7.2) | .20 |
BMI, body mass index.
At the time of the index VTE.
At 12 months after the index VTE.
The proportion of VTE recurrence was 11% (17/156) after 12 months and 17% (26/156) after 24 months. At 12 months, 5% of men had recurrent VTE compared with 19% of women (P = .02), 11% of patients with PE/proximal DVT compared with 11% of patients with distal DVT (P = 1.0), and 13% of patients with a D-dimer ≥1022 ng/mL compared with 9% in those with a value <1022 ng/mL (P = .61). At 24 months, 12% of men had recurrent VTE compared with 23% of women (P = .08), 17% of patients with PE/proximal DVT compared with 16% of patients with distal DVT (P = 1.0), and 18% of patients with a D-dimer ≥1022 ng/mL compared with 15% in those with a value <1022 ng/mL (P = .83).
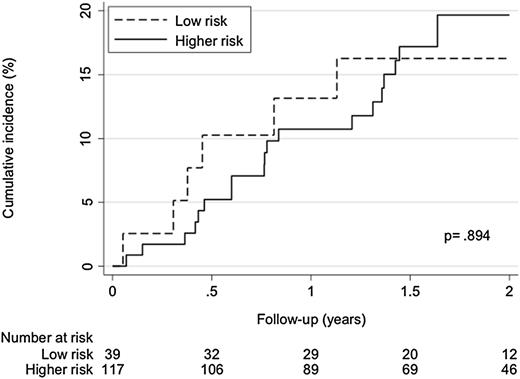
Based on the updated Vienna Prediction Model, patients with a predicted 12-month risk <6.2% were classified as low-risk. The proportion of recurrent VTE did not differ between low- vs higher-risk patients at 12 months (13% vs 10%; P = .77) and 24 months (15% vs 17%; P = 1.0). Cumulative incidence curves did not differ between the 2 groups (P = .89, Figure 1). The Hosmer–Lemeshow test indicated a suboptimal model fit at 12 and 24 months (P = .03 and P = .06, respectively). The area under the ROC curve for predicting VTE recurrence was 0.39 (95% confidence interval [CI], 0.25-0.52) at 12 months and 0.43 (95% CI, 0.31-0.54) at 24 months. The exclusion of patients with prior VTE (n = 23) did not change the results. When we assumed missing D-dimer values to be normal (379 ng/mL, median value of patients with a D-dimer <500 ng/mL) or abnormal (1147 ng/mL, median value of patients with a D-dimer ≥500 ng/mL) in a sensitivity analysis, the area under the ROC curve for predicting recurrent VTE at 12 months was 0.37 (95% CI, 0.26-0.48) and 0.40 (95% CI, 0.28-0.51), respectively, confirming the robustness of our results.
Kaplan–Meier curve for VTE recurrence in low- vs higher-risk patients. Low risk was defined as lowest quartile of predicted 12-month risk according to the updated Vienna Prediction Model.
Kaplan–Meier curve for VTE recurrence in low- vs higher-risk patients. Low risk was defined as lowest quartile of predicted 12-month risk according to the updated Vienna Prediction Model.
In our study of elderly patients with unprovoked VTE, the updated Vienna Prediction Model did not discriminate between patients who developed recurrent VTE and those who did not. Compared with the derivation population, our patients were older (median age, 74 vs 53 years) and had higher D-dimer levels (median, 1022 vs 356 ng/mL). Whether age itself is independently associated with VTE recurrence is controversial.3,4,7,13,14 It is possible that the higher D-dimer levels in elderly patients could decrease the accuracy of the model, which was derived in younger patients. Given that the increased recurrence risk in men has been demonstrated predominantly in younger patients (mean age, 45 to 68 years),4,9,15,16 it is uncertain whether sex is a risk factor for recurrence in the elderly.
Our work has limitations. First, our study was part of a prospective cohort of elderly patients with VTE, which was not primarily designed to validate the updated Vienna Prediction Model. Thus, our sample was relatively small and our study may not have sufficient power to detect a difference in VTE recurrence. Second, because we validated the model in the elderly, our results do not apply to younger patients. Third, 20 patients with unprovoked VTE had a recurrence between stopping AC and the start of follow-up, and were excluded from analysis (mostly because they were anticoagulated or had missing D-dimer values). Thus, we cannot exclude that the model would have performed differently if these patients had been included in our analysis. Finally, we used a quantitative ELISA-based D-dimer assay (VIDAS, bioMérieux) that may not be entirely comparable to the test used in the derivation study (Asserachrom D-dimer, Boehringer Mannheim).9
In conclusion, the updated Vienna Prediction Model may not be suitable for identifying elderly patients with unprovoked VTE who are at low risk of VTE recurrence. Further studies should attempt to develop an age-specific Vienna Prediction Model or to update the model, including age as a predictor.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank all collaborators of the SWITCO65+ study.
The study was supported by a grant from the Swiss National Science Foundation (SNSF) (33CSCO-122659/139470).
Authorship
Contribution: T.T., M.M., and A.L. were responsible for planning of the study, statistical analyses, and drafting of the manuscript; N.R. performed data collection, intellectual review of the manuscript, and obtained funding from the SNSF; and D.A. was the principal investigator and was responsible for planning of the study, data collection, drafting of the manuscript, and obtaining funding from the SNSF.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Tobias Tritschler, Department of General Internal Medicine, Bern University Hospital, Inselspital, 3010 Bern, Switzerland; e-mail: tobias.tritschler@insel.ch.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal