Abstract
Among mechanisms underlying cytotoxic drug resistance is activation of diverse DNA damage response (DDR) pathways. Poly(ADP-ribose) polymerases (PARP)-1/2 facilitate both single- and double-strand break (DSB) repair and play a key role in the base excision repair (BER) of chemotherapy-damaged DNA. The PARP inhibitor veliparib (V) potentiates the cytotoxicity of different chemotherapeutics, including temozolomide (TEM). TEM induces distinct alkylating events in neoplastic cells whose ultimate outcome depends on the interaction of BER, mismatch repair (MMR), O(6)-methylguanine-DNA methyltransferase (MGMT), and DSB repair. While clinical activity of TEM has been mainly observed in MGMT-deficient AML, V potentiated cytotoxicity of TEM in leukemia cells in vitro in the setting of MGMT overexpression or deficient MMR pathway (Mol Cancer Ther, 2009).
Methods: We conducted a Phase I study to determine maximum tolerated dose (MTD) and recommended Phase II dose (RP2D) of V+TEM, using a 3+3 dose escalation. Patients (pts) ≥60 years (yrs) with newly diagnosed poor cytogenetic-risk AML/ALL who were not candidates for intensive therapy, or ≥18 yrs with relapsed/refractory AML/ALL, secondary AML (therapy-related or arising from MDS or MPN), and CMMoL-2 were eligible. Any number of prior regimens, including allogeneic transplant (alloSCT), were allowed. V was given orally day (d)1 once, then twice a day on d4-12 at one of 6 dose levels (DL) (DL1A-B 20mg; DL2-DL3-DL4-DL5-DL6: 40-80-120-150-200 mg). TEM was given orally once a day on d3-9 (DL1A 150 mg/m2/d; DL1B-DL6 200 mg/m2/d). 28-day cycles (cy) were repeated depending on response/tolerability (4-6 weeks delay allowed) with V on d1-8 and TEM d1-5. TEM was taken on empty stomach with antiemetics and V was taken irrespective of meals.
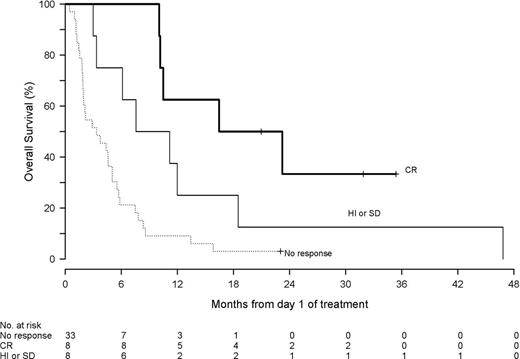
Results: Forty-nine pts with median age 69 yrs (range, 22-88; 47% ≥70) were treated. Of 47 AML pts, 29 (62%) had secondary AML and 27 (57%) adverse karyotype. Median number of prior treatments for AML was 1 (range, 0-6): 18 (38%) had median 1 prior therapy (range, 1-3) for MDS; 30 (64%), 9 (18%), 34 (69%) received hypomethylating agents, alloSCT and intensive chemotherapy, respectively. Overall 42 (85%) pts were refractory to their last treatment. Pts received a median of 1 (range, 1-7) cy of therapy. Two did not complete cy 1, pt withdrawal d5 and progressive fungal pneumonia d9 with death d15 of progressive disease (PD). The MTD/RP2D was defined at V 150 mg and TEM 200 mg/m2; 2 of 4 pts treated at V 200 mg and TEM 200 mg/m2 developed dose-limiting toxicity of grade (gr) 3 oral mucositis/esophagitis. The most frequent drug-related toxicities (NCI CTC v4) were gr 1/2 nausea/vomiting (39%), fatigue (26%), oropharyngeal mucositis (26%), constipation (12%), and diarrhea (10%). Other common toxicities were infectious, including febrile neutropenia (29%), pneumonia (20%), bacteremia (18%). One (2%) pt died ≤d30 and 12 (24%) ≤d60 mainly of PD (1 pt fungal pneumonia before count recovery d31). Overall response rate was 33% (complete remission (CR), hematologic improvement (HI)/stable disease) with 8 (16%) pts achieving CR (1 CRi). Median overall survival was 5.03 months, for all responders 11.58 months, and for CR pts 19.89 months (Fig 1). Responses occurred at all DLs. Three CR pts underwent alloSCT; 2 remain in CR at ~3 yrs.
Pharmacokinetics (PK): V or TEM PKs were not altered with co-administration. There was a correlation between the DLT of mucositis and V single (Cmax P=0.005; AUC P=0.009) and multiple dose exposure (Cmax P = 0.02; AUC P=0.03).
Pharmacodynamics and pharmacoepigenetics: Four of 39 pts examined had MGMT methylation (3 CR; 75%) and 2 had BRCA-1 methylation (1 HI) in peripheral blood (PB) or bone marrow (BM) mononuclear cells (MC). Defective FancD2 pathway was observed in the BMMC of 19/19 pts using FancD2 ubiquitylation assays but did not correlate with response. V reduced PAR levels by >75% in PBMC of most pts and in the presence of TEM. Induction of γ-H2AX in CD34+ cells was seen upon V/V+TEM treatment.
Conclusion: V plus TEM demonstrated safety and activity in this resistant and elderly leukemia population. Response rate was higher in MGMT methylated pts, but responses were also seen in pts who had no MGMT methylation, had failed multiple therapies, had secondary AML and/or adverse karyotype. Future clinical study should aim to identify pts with defective DDR pathways who are most likely to respond to this therapeutic approach.
Off Label Use: Temozolomide is not approved for AML. Beumer:Millenium: Other: Research support. Gore:Celgene: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal