Abstract

Background: Myelodysplastic syndromes (MDS) are clonal hematological diseases which present with cytopenias. Hematopoietic cell transplantation is usually limited to fit patients with higher risk MDS and donor availability. Hypomethylating agents (azacitidine and decitabine) have been the mainstay option for the management of MDS with different clinical efficacy in low versus high risk MDS trials. No trials have compared the two agents.
Aim: To conduct a systematic review and network analysis comparing the efficacy of azacitidine to decitabine.
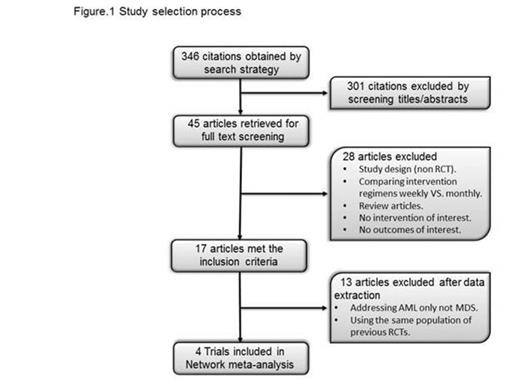
Methods: The protocol of the systematic review was developed a priori. A comprehensive search of several databases (MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, and Scopus) was conducted from each database's earliest inception through November 20th, 2014 without language restrictions. Trials enrolling adults diagnosed with MDS who received hypomethylating agents (azacitidine or decitabine) therapy were included. Studies were screened by two independent reviewers and differences were resolved by consensus. The Cochrane Risk of bias tool was used to appraise the trials. Random effects model was used to pool relative risks (RR) of outcomes (overall survival, overall response rate, hematologic improvement and grade 3 or 4 toxicity). Adjusted indirect comparisons were used to estimate RR for indirect comparisons (Glenny AM, et al. Health Technol Assess. 2005). All statistical analyses were conducted using STATA, version 13 (StataCorp LP, College Station, TX).
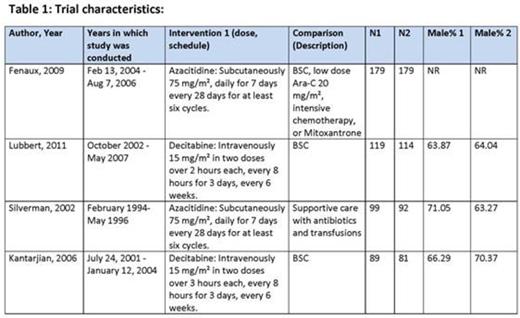
Results: Only four trials met the eligibility criteria (Figure 1). Two trials compared Azacitidine (75mg/m²/day SC x 7 days) to the best suppurative care (BSC) and included 549 patients (278 azacitidine and 271 BSC, age average: 69; range: 31-92), and the other 2 compared decitabine (15 mg/m² IV q 8 hours x9) to BSC and included 403 patients (208 Decitabine and 195 BSC, age average: 69.7; range: 60-90) (Table 1). The proportion of patients with intermediate-2 and high-risk myelodysplastic syndrome (based on International Prognostic Scoring System (IPSS)) in trials comparing decitabine to BSC was 82.21% and 83.08%; respectively, and in trials comparing azacitidine to BSC was 62.59% and 61.26%; respectively. The risk of bias was moderate overall. Compared to BSC, azacitidine was significantly associated with lower risk of death (RR=0.83, 95% CI: 0.74-0.94, p=0.002) whereas the effect of decitabine did not reach statistical significance (RR=0.88, 95% CI: 0.77-1.001, p=0.053). Both drugs were superior to BSC in terms of partial and complete response. Head to head comparisons were not statistically significant (except for the outcome of complete response where low certainty evidence suggested that azacitidine treated patients were less likely to have complete response compared to decitabine (RR=0.11, 95% CI= 0.01, 0.86, p=0.04). (Table 2).
Conclusion: Azacitidine and decitabine are both superior to BSC. The available indirect evidence comparing the two agents warrants low certainty and cannot reliably confirm superiority of either agent. Head-to-head trials are needed. In the meantime, the choice of agent should be driven by patients' preferences, drug availability and cost.
Results of meta-analysis
| Outcome . | Azacitidine VS. Decitabine . | Azacitidine VS. BSC . | Decitabine VS. BSC . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | LCI | HCI | P value | RR | LCI | HCI | P value | RR | LCI | HCI | P value | |
| Death | 0.95 | 0.79 | 1.13 | 0.54 | 0.83 | 0.74 | 0.94 | 0.002 | 0.88 | 0.77 | 1.001 | 0.05 |
| Complete response | 0.11 | 0.01 | 0.86 | 0.04* | 2.56 | 1.44 | 4.58 | 0.001 | 23.46 | 3.22 | 170.84 | 0.002 |
| Partial response | 0.35 | 0.04 | 3.03 | 0.34 | 4.91 | 2.27 | 10.63 | <0.0001 | 14.02 | 1.87 | 105.08 | 0.01 |
| Major erythroid improvement | 0.47 | 0.03 | 8.37 | 0.60 | 6.37 | 3.93 | 10.33 | <0.0001 | 13.67 | 0.79 | 235.57 | 0.07 |
| Major platelet improvement | 1.51 | 0.30 | 7.56 | 0.62 | 4.80 | 2.98 | 7.70 | <0.0001 | 3.19 | 0.68 | 14.89 | 0.14 |
| Major neutrophil improvement | 2.89 | 0.56 | 14.82 | 0.20 | 2.63 | 1.68 | 4.12 | <0.0001 | 0.91 | 0.19 | 4.38 | 0.907 |
| Hematologic improvement | 0.25 | 0.06 | 1.09 | 0.07 | 2.18 | 1.67 | 2.85 | <0.0001 | 8.62 | 2.05 | 36.32 | 0.003 |
| Anemia | 1.18 | 0.53 | 2.63 | 0.69 | 0.89 | 0.75 | 1.06 | 0.198 | 0.76 | 0.35 | 1.66 | 0.49 |
| Neutropenia | 0.99 | 0.75 | 1.30 | 0.92 | 1.87 | 1.63 | 2.14 | <0.0001 | 1.90 | 1.49 | 2.42 | <0.0001 |
| Thrombocytopenia | 0.87 | 0.64 | 1.18 | 0.37 | 1.63 | 1.43 | 1.86 | <0.0001 | 1.87 | 1.43 | 2.45 | <0.0001 |
| Infection | 1.13 | 0.52 | 2.43 | 0.76 | 1.25 | 0.60 | 2.60 | 0.55 | 1.11 | 0.87 | 1.42 | 0.41 |
| Outcome . | Azacitidine VS. Decitabine . | Azacitidine VS. BSC . | Decitabine VS. BSC . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | LCI | HCI | P value | RR | LCI | HCI | P value | RR | LCI | HCI | P value | |
| Death | 0.95 | 0.79 | 1.13 | 0.54 | 0.83 | 0.74 | 0.94 | 0.002 | 0.88 | 0.77 | 1.001 | 0.05 |
| Complete response | 0.11 | 0.01 | 0.86 | 0.04* | 2.56 | 1.44 | 4.58 | 0.001 | 23.46 | 3.22 | 170.84 | 0.002 |
| Partial response | 0.35 | 0.04 | 3.03 | 0.34 | 4.91 | 2.27 | 10.63 | <0.0001 | 14.02 | 1.87 | 105.08 | 0.01 |
| Major erythroid improvement | 0.47 | 0.03 | 8.37 | 0.60 | 6.37 | 3.93 | 10.33 | <0.0001 | 13.67 | 0.79 | 235.57 | 0.07 |
| Major platelet improvement | 1.51 | 0.30 | 7.56 | 0.62 | 4.80 | 2.98 | 7.70 | <0.0001 | 3.19 | 0.68 | 14.89 | 0.14 |
| Major neutrophil improvement | 2.89 | 0.56 | 14.82 | 0.20 | 2.63 | 1.68 | 4.12 | <0.0001 | 0.91 | 0.19 | 4.38 | 0.907 |
| Hematologic improvement | 0.25 | 0.06 | 1.09 | 0.07 | 2.18 | 1.67 | 2.85 | <0.0001 | 8.62 | 2.05 | 36.32 | 0.003 |
| Anemia | 1.18 | 0.53 | 2.63 | 0.69 | 0.89 | 0.75 | 1.06 | 0.198 | 0.76 | 0.35 | 1.66 | 0.49 |
| Neutropenia | 0.99 | 0.75 | 1.30 | 0.92 | 1.87 | 1.63 | 2.14 | <0.0001 | 1.90 | 1.49 | 2.42 | <0.0001 |
| Thrombocytopenia | 0.87 | 0.64 | 1.18 | 0.37 | 1.63 | 1.43 | 1.86 | <0.0001 | 1.87 | 1.43 | 2.45 | <0.0001 |
| Infection | 1.13 | 0.52 | 2.43 | 0.76 | 1.25 | 0.60 | 2.60 | 0.55 | 1.11 | 0.87 | 1.42 | 0.41 |
*These results warrant low certainty due to imprecision (very small number of events) and are driven by 14 patients achieving complete response in BSC arm in one trial.
Al-Kali:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal