Abstract

Relapse of hematologic malignancies remains a major cause of treatment failure and mortality among patients receiving allogeneic hematopoietic cell transplantation (HCT). Patients relapsing after a matched related or unrelated donor transplantation may benefit from donor lymphocyte infusion (DLI) as part of their post relapse therapy. DLI post-relapse has less frequently been utilized among recipients of HIDT presumably due to the potential for severe GVHD if high T-cell doss are administered without immunosuppression. However, reluctance to administer DLI may limit the possibility of remission following disease relapse in HIDT. We compared the frequency of use of DLI and survival outcomes for patients relapsing after HIDT using post-transplant cyclophosphamide to those relapsing after MRD or MUD HCT at our institution.
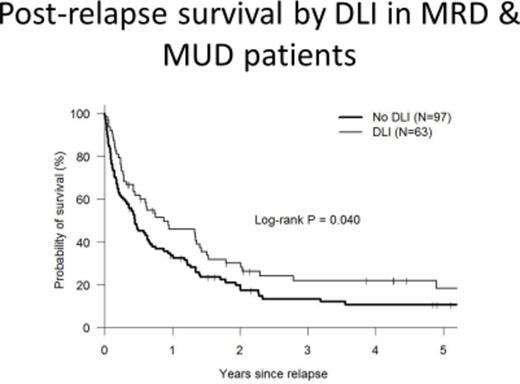
195 consecutive HCT recipients with relapse of hematologic malignancy occurring after HIDT (N=35), MUD (N=74) and MRD (N=81) between 1998 and 2014 were included in this analysis. The median age was 50 years (19-77 years) and median time to relapse was 159 days (25-2465 days) post HCT. Patients receiving HIDT had similar median time to relapse (5.1 vs 5.2 vs 5.2 months, p=0.638), Dana-Farber/CIBMTR disease risk index (DRI), comorbidity index (CMI) scores, longer times to neutrophil engraftment (17 vs 14 vs 14 days, p<0.001), and platelet engraftment (28 vs 19 vs 18 days, p<0.001) when compared to MUD and MRD recipients respectively. Post-relapse survival at 1 year was worse among HIDT recipients when compared to MRD (9% versus 41%, p=0.008) and MUD (9% vs 35%, p=0.025). DLI was used in 3 (8%) relapsed HIDT patients, 48 MRD patients (59%) and 28 (38%) MUD recipients. Among patients relapsing post MRD and MUD HCT, use of DLI was associated with a better post relapse survival (p=0.04). In a multivariate analysis, donor type (HIDT), time to relapse (<3 months versus > 3months post-transplant) and comorbidity index (CMI score >= 3) were all predictive of worse post relapse survival.
This analysis shows that relapse post HIDT carries a worse prognosis than relapse post MRD and MUD. Efforts such as post-transplant maintenance and haploidentical DLI infusions should be investigated further in the HIDT setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal