Abstract
INTRODUCTION In newly diagnosed Multiple Myeloma (MM) patients (pts), Copy Number (CN) losses of chromosome 17p13, carrying the TP53 tumor-suppressor gene, are strong predictors of poor outcomes. On the contrary, the prognostic relevance of TP53 mutations at the onset of the disease is less clear, due to the very limited frequency of clonal lesions, as revealed by Sanger sequencing. To address this poorly investigated issue, we used an ultra-deep sequencing (UDS) approach to characterize the TP53 structural architecture in both newly diagnosed and relapsed MM pts and to assess the prognostic role and evolution over time of small TP53 mutated sub-clones.
SAMPLES AND METHODS A cohort of 99 newly diagnosed MM pts treated up-front with bortezomib-based regimens and autologous stem cell transplantation, was included in this molecular study. In 29 cases, samples were collected both at diagnosis and at relapse(s). DNA was obtained from CD138+ highly purified plasma cells. TP53 gene mutational status was analysed by using an amplicon-targeted UDS approach (GSJ, 454 Roche Life Sciences). In order to discriminate between low frequency sub-clonal TP53 variants and sequencing errors, sequencing raw data were filtered according to cut-off values based on different ranges of sequences' coverage depth. Additional filters were also applied, based on both quality and biological cut-offs, to obtain a final confident list of variants. Analysis of CN alterations (CNAs) was performed by SNPs array and results analysed with ChAS software.
RESULTS With a median coverage of 1386X, a list of 129 correctly called TP53 variants (either missense, or nonsense or splice ones), including 20 INDELs, was detected. Only deleterious and N/A variants (according to SIFT classification) were included in the list. Most newly diagnosed MM pts (55%) carried at least one TP53 sub-clonal variant (on average 1.08 variants per pts), with 45/99 (45%) carrying non-mutated TP53. Pts carrying TP53 sub-clonal variants bared also TP53 CN hemizygous losses (20%), CKS1B gains (56%) and cdkn2c losses (14%). According to TP53 sub-clonal mutational load, pts were stratified in two sub-groups, including 28 pts with ≥2 (high load) and 71 with <2 variants (low load), respectively. Eleven out of 129 variants were recurrent (RVs), as being detected in at least 3% of pts, with Variants Allele Frequencies (VAFs) ranging from 0.24 to 70.1% (median 0,53%); RVs were observed in 29 pts.
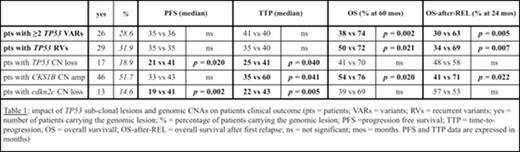
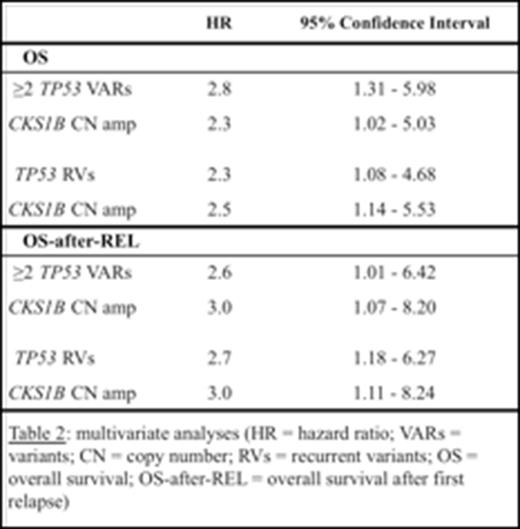
The clinical impact of the TP53 sub-clonal mutational load, as well as of variants recurrence, was evaluated in 90/99 MM (median follow up = 70 months). Results of statistical analysis are summarized in Table 1. Pts carrying either high TP53 sub-clonal mutational load or RVs had significantly shorter OS and OS after relapse, as compared to the others, while no difference between these two groups was seen regarding PFS and TTP. Multivariate analysis showed that high TP53 mutational load, as well as the presence of TP53 RVs, both resulted independent factors adversely affecting OS and OS after relapse (Table 2). Of note, none of the detected genomic aberrations significantly influenced the response to front-line induction therapy.
The distribution of both TP53 sub-clonal variants and genomic CNAs was overall modified in samples collected at relapse(s): 90% of relapsed pts carried at least one sub-clonal variant (on average 1.63 variants per pts) with 3/29 (10%) relapsed MM carrying non-mutated TP53. Moreover, 5 different sub-clonal lesions proved a linear increment of both TP53 VAFs (from 29.4% to 54.6%; from 7.8% to 12.4%; from 0.5% to 4.3%) and TP53 CN loss smooth signal (from 7% to 89% and from 50% to 100%), as evaluated in longitudinally collected samples.
CONCLUSIONS The UDS analysis of TP53 coding sequence in newly diagnosed MM highlighted for the first time a high rate of variants, recurring with a wide range of frequencies among samples. The increased number of TP53 sub-clonal variants per pts in samples collected at relapse(s), compared to that seen at the onset of the disease, suggests a sub-clonal dynamics over time. This finding might explain the adverse impact of high TP53 sub-clonal mutational load and TP53 RVs on OS, due to a shorter OS after relapse.
Acknowledgments: Roche Diagnostics for applicationsupport in the realization of this project.
Zamagni:Celgene Corporation: Honoraria, Speakers Bureau; Janssen Pharmaceuticals: Honoraria, Speakers Bureau; Amgen: Honoraria, Speakers Bureau. Martinelli:Novartis: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau; Ariad: Consultancy; AMGEN: Consultancy; ROCHE: Consultancy; Pfizer: Consultancy; MSD: Consultancy. Cavo:Janssen-Cilag, Celgene, Amgen, BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal