Abstract
Pro-survival molecules including BCL-2 play critical roles in leukemia transformation and chemoresistance. ABT-199/GDC-0199 (venetoclax) is an orally available BH3-mimetic that binds with high affinity to BCL-2, but lacks affinity for BCL-XL and MCL-1. We have recently demonstrated anti-leukemia potency of venetoclax in acute myeloid leukemia (AML) models (Pan et al. Cancer Discovery 2014). However, venetoclax poorly inhibits MCL-1, causing resistance in leukemia cells that rely on MCL-1 for survival. The RAF/MEK/ERK (MAPK) cascade is a major effector pathway in AML that is activated by upstream mutant proteins such as FLT3, KIT and RAS. Additionally, the MAPK pathway regulates BCL-2 family proteins by stabilizing anti-apoptotic MCL-1 and inactivating pro-apoptotic BIM. In this study, we evaluated the anti-tumor effects of concomitant BCL-2 and MAPK blockade by venetoclax in combination with MEK1/2 inhibitor GDC-0973 (cobimetinib)..
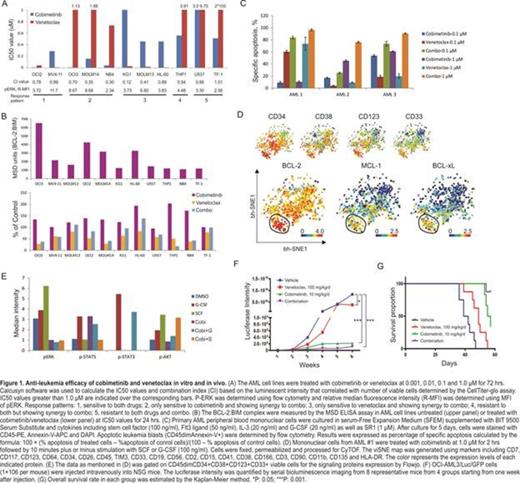
We initially examined activity of these agents in a panel of myeloid leukemia cell lines with diverse genetic alterations (Fig. 1A). The IC50 values of cobimetinib ranged from < 0.01 µM to > 1 µM after 72 hours of drug treatment but did not correlate with the basal level of p-ERK1/2. In 7 out of 11 cell lines, combination of the agents elicited synergistic growth inhibition. Notably synergism of venetoclax with cobimetinib was observed in venetoclax-resistant cell lines (MOLM14, OCI-AML3, NB4 and THP1). Ongoing analysis of pharmacodynamic markers include transcriptome assessment by RNA sequencing, functional proteomics by reverse phase protein array (RPPA) and quantification of BCL-2:BIM and MCL-1:BIM complexes using the electrochemiluminescent ELISA assay (Meso Scale Discovery, MSD-ELISA). The preliminary MSD data revealed that BCL-2:BIM complex was disrupted in most cell lines and accumulated following cobimetinib treatment, which may be due to the disruption of MCL-1:BIM complex by inhibition of MEK (Fig. 1B).
In a long-term culture of primary AML blasts in serum-free stem cell growth medium supplemented with cytokines and StemRegenin 1 (SR1) to main the immature state of leukemia cells, the combination of venetoclax and cobimetinib induced distinct apoptotic cell death, with AML #1 sensitive to venetoclax but resistant to cobimetinib. Alternatively, AML #2 and #3 samples were resistant to venetoclax but sensitive to cobimetinib and the combination of both drugs (Fig. 1C). We next investigated signaling patterns and BCL-2 family protein expression in AML stem/progenitor cells using a 34-antibody panel and time-of-flight mass cytometry (CyTOF). In AML#1, BCL-2 was expressed in leukemia blasts, with enrichment in a progenitor AML population phenotypically defined as CD45dim CD34+ CD38+ CD123+ CD33+ (Fig. 1D). The high expression level of BCL-2 and low expression of MCL-1 and BCL-XL may account for sensitivity to venetoclax in AML#1. Both basal and G-CSF- or SCF-stimulated p-ERK was efficiently down-regulated by cobimetinib; however, G-CSF-evoked p-STAT3/5 and SCF-induced p-AKT were only slightly reduced (Fig. 1E). Notably we observed increased phosphorylation of STAT5 pathway upon treatment with cobimetinib, suggesting that active MAPK signals inhibit phosphorylation of the JAK-STAT pathway, as previously reported (Krasilnikov et al. Oncogene, 2003 and Lee at al. Cancer Cell, 2014).
To test the efficacy of both compounds in vivo, we injected NSG mice with genetically engineered OCI-AML3/Luc/GFP cells. Bioluminescent imaging (BLI) demonstrated significantly reduced leukemia burden in treated groups compared to controls, more prominently in the cobimetinib single agent and venetoclax plus cobimetinib co-treated mice (Fig. 1F). The efficacy study is ongoing and median survival for cobimetinib and venetoclax co-treated mice has yet to be determined (Fig. 1G).
In summary, our data demonstrates that combinatorial blockade of MAPK and BCL-2 pathways is synergistic in the majority of AML cell lines tested and can overcome intrinsic resistance to venetoclax. Ongoing studies will evaluate efficacy of this combination therapy in primary human AML xenografts and elucidate mechanisms of synergy.
Leverson:AbbVie: Employment, Equity Ownership. Dail:Genentech: Employment, Equity Ownership. Phillips:AbbVie: Employment, Other: Shareholder, Patents & Royalties. Chen:Abbvie: Employment, Equity Ownership. Jin:Abbvie: Employment, Equity Ownership. Jabbour:Pfizer: Consultancy, Research Funding. Sampath:Genentech: Employment, Equity Ownership. Konopleva:Novartis: Research Funding; AbbVie: Research Funding; Stemline: Research Funding; Calithera: Research Funding; Threshold: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal