Abstract
Background:
The standard therapy for primary gastric diffuse large B-cell lymphoma (DLBCL) is chemotherapy of R-CHOP with/without involved-field radiation therapy. Although some reports indicated that gastrointestinal complications after chemotherapy for DLBCL occur at a rate of 0-26%, little is known about riskfactors for the complications. In addition, to detect DLBCL in gastric lesion, both of positron emission tomography-computed tomography (PET-CT) and esophagogastroduodenoscopy (EGD) are useful tools. However, there have been few reports comparing them. The aim of this study is to show the outcomes including treatment-related complications in patients with gastric DLBCL and risk factors for the gastric complications. Moreover, we evaluated whether PET-CT is sufficient to detect DLBCL in gastric lesion by comparing with EGD.
Patients and methods:
This retrospective study included consecutive patients with newly diagnosed DLBCL between October 2003 and July 2014 who underwent EGD and were treated with R-CHOP in our hospital. We classified the patients into three groups. Group A-1: patients who had documented DLBCL in gastric lesion by EGD and underwent PET-CT; group A-2: patients who had documented DLBCL in gastric lesion by EGD and did not underwent PET-CT; group B: patients who had no documented DLBCL in gastric lesion by EGD and underwent PET-CT. Suspected lymphomatous lesions by EGD were biopsied and immunopathologically examined. Gastric DLBCL was defined only when pathologically confirmed. In PET-CT, gastric lesions with SUV max ≥ 5 were considered positive. Outcomes and risk factors for complications among group A were analyzed using the logistic regression model. We evaluated significance of PET-CT and EGD in group A-1 and B by the positive predictive value (PPV) and the negative predictive value (NPV).
Results:
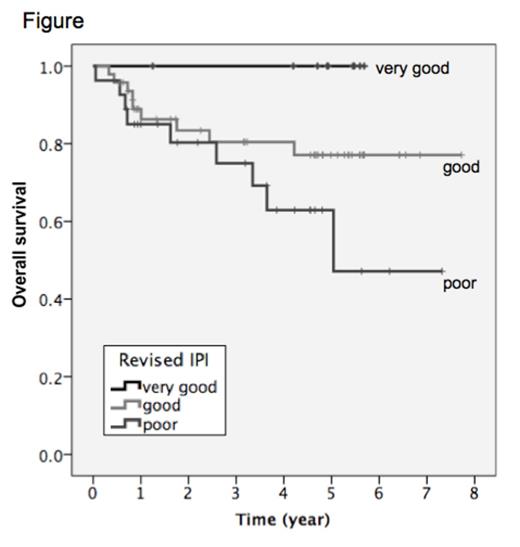
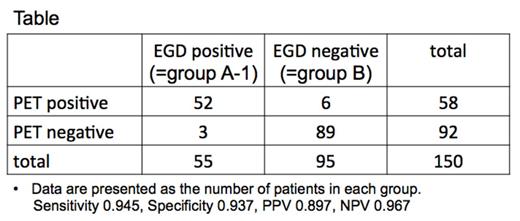
Among 448 patients diagnosed with DLBCL, 178 patients were enrolled for our study: 55 in group A-1, 28 in group A-2 and 95 in group B. Among 83 patients with gastric DLBCL (group A), the median age was 69 years (range, 29-85). The numbers of patients with clinical stage (Ann Arbor classification) I, II, III, and IV were 27, 18, 5, and 33, respectively. The rate of complete remission was 87%, and the median 3- and 5-year over survival (OS) were 81% and 75%, respectively. The median 3-year OS of patients with very good, good, and poor grade of Revised International Prognostic Index (R-IPI) was 100%, 77%, and 63%, respectively (Figure, p=0.025). Ten patients had gastric complications: 6 with bleeding that needed blood transfusion and 3 with gastrointestinal stenosis defined as ordinary endoscopy could not pass, no patients had gastrointestinal perforation. Most of bleeding (66.7%) occurred during the first cycle of R-CHOP (median, 15 days; range, 1-206). A multivariate analysis showed that low serum albumin (ALB) at diagnosis was an independent risk factor for gastric complications (odds ratio 10.75, p <0.001). The numbers of patients with positive or negative results examined by PET-CT or EGD in group A-1 and B were shown in Table. PPV and NPV of PET-CT were 0.90 and 0.97, respectively.
Conclusions:
The present study showed that R-IPI was also predictive of survival in gastric DLBCL and low ALB at diagnosis as a significant risk factor for gastric complications following R-CHOP. In addition, our data suggested that PET-CT may be sufficient in the role of detecting gastric lesion of DLBCL because of high PPV and NPV.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal