Abstract
Introduction: Experimental and clinical data have shown that iron overload (IO) has the potential to accelerate progression of myelodysplastic syndromes (MDS) towards secondary leukemia and coincides with a lower survival rate. While genetic instability is understood as a common driver of MDS progression, the mechanisms involved have not yet been fully explored, albeit that oxidative stress is considered to be a main factor for IO related genetic instability. We aimed to investigate the influence of IO, measured by serum ferritin (SF) as a suitable surrogate parameter, on the stability of the genome of MDS patients (pts).
Patients/Methods: 60 pts with proven MDS were included, cut-off for elevated SF being 275 µg/l. 29 pts had normal SF levels (median 61 µg/l [range 8-256 µg/l]), 31 pts had elevated SF levels (median 1,246 µg/l [283-6,907]); 1 out of 8 patients with SF > 1,005 µg/l tested positive for labile plasma iron (LPI). Pts were investigated for possible correlations of IO with distinct manifestations of genetic instability as shown by TP53 mutations, chromosome banding analysis, and molecular karyotyping (SNP array analysis). DNA double-strand breaks were quantified by γH2AX immunostaining on enriched CD34+ peripheral blood cells (PB). In addition, telomere length (TL) in PB granulocytes and lymphocytes was analyzed using flow-FISH, PB of 104 healthy donors being used for age-adaption. Plasma nitric oxide metabolites (nitrite, nitrate, nitroso species) are pending but will be screened for a possible correlation with SF.
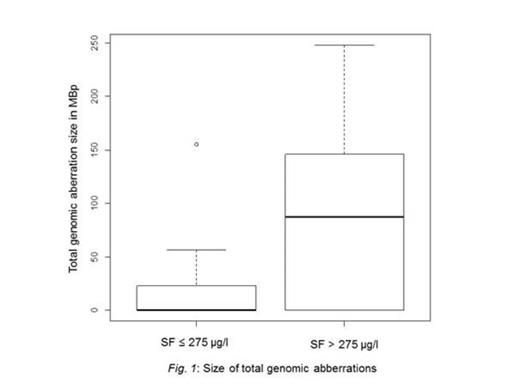
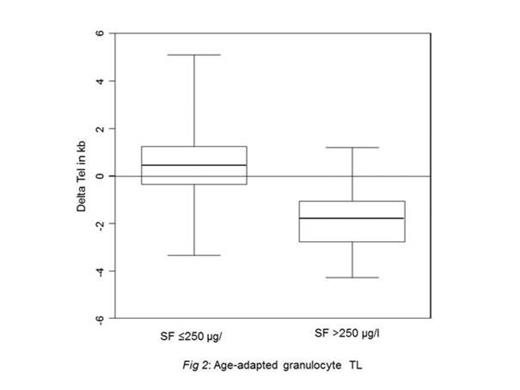
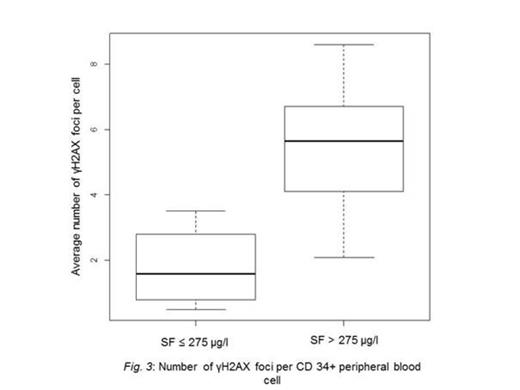
Results: Parameters for genomic stability were determined in the group of pts with elevated SF levels and the group of pts with normal SF levels. Through SNP array analysis, pts with increased SF levels were found to have significantly bigger total genomic aberrations (TGA) size than the subgroup with normal SF levels (median 87.5 Mbp TGA [range 0-229] vs. 0 Mbp TGA [0-155]; p = 0.005; Fig. 1). Likewise, telomere analysis showed significant more age-adapted TL shortening in granulocytes, representing the myeloid compartment, in the subgroup with increased SF levels (mean -1.81 kb) compared to patients with normal SF (0,64 kb, p = 0.003; Fig. 2). No significant TL shortening in lymphocytes of pts with normal SF was observed compared to pts with elevated SF. When only pts with marrow blasts <10% were considered, the subgroup with increased SF levels exhibited higher numbers of γH2AX-foci per CD34+ cell (median 5.7 γH2AX foci [range 2.1-8.6] vs. 1.6 γH2AX foci [0.5-3.5]; p = 0.008; Fig. 3). Elevated SF levels had no impact on the number, or type of chromosome abnormalities. Sanger sequencing identified only one patient with a TP53 mutation (SF = 1,246 µg/l); a search for smaller TP53-mutated clones by ultra-deep-sequencing is under way.
Conclusion: In this MDS cohort, higher SF levels were significantly associated with bigger TGA size, premature granulocyte TL shortening, and increased numbers of γH2AX foci in CD34+ cells. These results further support the assumption that IO might be causally related to genetic instability in pts with MDS. Furthermore, our data suggest that SF levels not only above 1,000 µg/l, but also between upper limit of normal value but below 1,000 µg/L adversely affect genetic stability. Additionally, our results imply that the biological relevance of LPI for IO in MDS might be overestimated and is in need of reevaluation. Therefore, iron chelation might be relevant for pts with MDS at lower SF levels than previously thought. Whether investigation of the level of genetic instability by comprehensive genomic analysis as indicated above may be beneficial for the therapeutic decision regarding the timing of iron chelation therapy in individual pts with MDS remains to be explored.
Al-Ali:Celgene: Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Brümmendorf:Bristol Myers Squibb: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria, Research Funding; Ariad: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Patents & Royalties: Patent on the use of imatinib and hypusination inhibitors, Research Funding. Gattermann:Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal