Abstract
Introduction
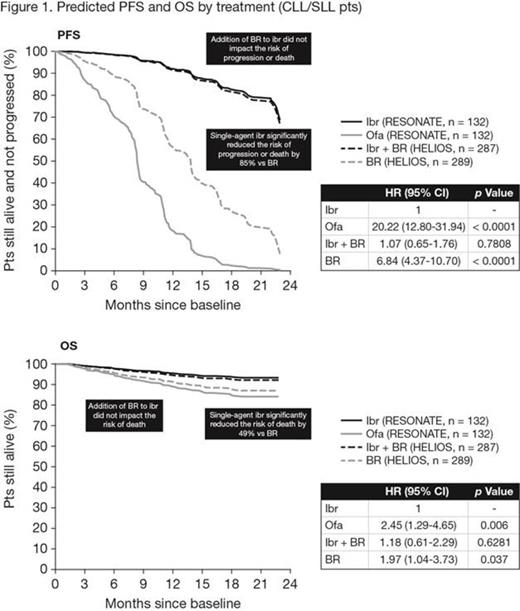
In 2 large phase 3 trials of patients (pts) with relapsed or refractory (R/R) CLL/SLL, single-agent ibrutinib (ibr) was superior to ofatumumab (ofa) (RESONATE; Byrd. NEJM 2013) and ibr + BR was superior to placebo + BR (HELIOS; Chanan-Khan. ASCO 2015). Both studies evaluated ibr in different pt populations with different relevant comparators (eg, ofa in pts who had relapsed following prior anti-CD20-based chemoimmunotherapy [CIT] and/or with del17p, and BR in pts eligible for CIT). In the absence of head-to-head evaluations of single-agent ibr vs BR or single-agent ibr vs ibr + BR, indirect comparisons can be used for hypothesis testing by potentially providing insights on the relative efficacy of treatments. As such, an indirect comparative analysis of data from RESONATE and HELIOS was performed. Recognizing biases inherent in cross-trial comparisons, including lack of randomization across trials and consequent differences in distributions of important confounding variables (eg, pt characteristics, prognostic factors), we used pt-level data from both studies to risk adjust for confounders using accepted multivariate statistical approaches.
Methods
In RESONATE, pts received 420 mg oral ibr daily until disease progression or unacceptable toxicity or intravenous ofa for up to 24 weeks. The primary end point was IRC-assessed PFS, with secondary end points of OS and ORR. In HELIOS, pts received BR (≤ 6 cycles) with either 420 mg oral ibr daily or placebo until disease progression or unacceptable toxicity. Pts with del17p were excluded. The primary end point was IRC-assessed PFS, with secondary end points of ORR and OS. Per protocol amendment in both studies, pts in comparator arms could switch to ibr upon IRC-confirmed progression. The current exploratory analysis was based on the latest available data from each trial (median time on study: RESONATE, 19 months; HELIOS, 17 months) using investigator assessments, but excluding del17p pts from RESONATE. Analyses were performed using data from both the overall CLL/SLL population and only the CLL pts. Separate multivariate Cox proportional hazards models were constructed for PFS and OS, including treatment and clinically relevant prognostic variables as covariates (age, gender, Rai staging, ECOG score, del11q status, refractory status, number of prior lines of therapy, bulky disease, IgVH status). Adjusted HRs and 95% CIs are presented vs single-agent ibr, along with predicted survival curves derived from the multivariate Cox regressions.
Results
RESONATE and HELIOS enrolled populations with notable differences making naïve comparison flawed. Because HELIOS enrolled only CIT-eligible pts, the trial included younger pts who had received fewer lines of therapy, as well as lower proportions of pts with purine analog refractory disease, del11q, or Rai stage 4 disease. These factors have been previously reported to influence outcomes in pts with R/R CLL/SLL and thus were included as covariates in the statistical models. Other baseline factors (gender, ECOG score, bulky disease, and IgVH status) were not notably different between the trials, but were found to impact PFS and OS and thus were included as additional covariates. In the overall CLL/SLL population, PFS and OS were comparable for single-agent ibr vs ibr + BR, and were significantly improved for single-agent ibr vs BR (Figure 1). Results for only the CLL pts were similar to those shown in Figure 1 for both PFS (ibr + BR vs single-agent ibr: 1.03 [0.61-1.75], p = 0.9042; BR vs single-agent ibr: 7.52 [4.72-11.99], p < 0.0001; single-agent ibr reduced the risk of progression/death by 87% vs BR) and OS (ibr + BR vs single-agent ibr: 1.20 [0.59-2.43], p = 0.6197; BR vs single-agent ibr: 2.24 [1.14-4.40], p = 0.0197; single-agent ibr reduced the risk of death by 55% vs BR).
Conclusions
The adjusted indirect comparisons reported here suggest superiority of single-agent ibr over BR for PFS and OS in patients with R/R CLL/SLL. The comparisons also suggest that the addition of BR to ibr did not improve PFS or OS compared with single-agent ibr. However, as median PFS has not been reached for either ibr arm, it is too early to draw firm conclusions. Longer follow-up in the ibr arms of these studies will be required to give an indication of whether CIT adds any benefit to ibrutinib for PFS and OS. Overall, these findings provide support for single-agent ibr as an appropriate choice for all pts with previously treated CLL/SLL.
Hillmen:Roche Pharmaceuticals: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Gilead: Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Celgene: Research Funding; Pharmacyclics LLC, an AbbVie Company: Honoraria, Research Funding. Fraser:Janssen: Honoraria, Research Funding, Speakers Bureau; Hoffman LaRoche: Consultancy, Honoraria; Celgene: Honoraria, Research Funding. Jones:Acerta Pharma BV: Research Funding. Rule:Roche: Consultancy, Other: Travel reimbursement; J&J: Consultancy, Other: Travel reimbursement, Research Funding; Celgene: Consultancy, Other: Travel reimbursement; Gilead: Research Funding. Dilhuydy:Roche: Honoraria, Other: Travel reimbursement; Janssen: Honoraria, Other: Travel reimbursement; Mundipharma: Honoraria. Jaeger:Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Cymbalista:Karyopharm: Honoraria; Roche: Honoraria; Gilead: Honoraria; Janssen: Honoraria, Research Funding. Sun:Janssen/J&J: Employment, Equity Ownership. Ninomoto:Pharmacyclics LLC, an AbbVie Company: Employment. Mahler:Janssen: Employment, Other: Travel reimbursement. Cheng:Pharmacyclics LLC, an AbbVie Company: Employment. Diels:Janssen: Employment. Clow:Pharmacyclics LLC, an AbbVie Company: Employment. Salman:Janssen/J&J: Employment, Equity Ownership. James:Pharmacyclics LLC, an AbbVie Company: Employment. Howes:Janssen/J&J: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal