Abstract
INTRODUCTION. Although remarkable advances have been reported in Multiple Myeloma (MM) therapy, mainly due to the introduction of novel agents, the disease remains incurable in most of the patients. The iperactivation of self-renewal mechanisms, like Hedgehog (Hh) pathway, which controls the refuel of the tumor clone, might be critical to disease recurrence. Whilst several studies suggestthatHh pathway is activated in the putative CD138- Myeloma Propagating Cells (MPCs), it is likely that also terminally differentiated CD138+ plasma cells might contribute to drug resistance, by reverting to an immature phenotype.
AIM. In order to dissect the role played by Hh pathway in different MM cells compartments, and to evaluate the impact of Hh pathway expression on patientsÕ clinical outcomes, a high-throughput molecular characterization was employed to explore the transcriptomic and genomic profiles in both CD138+ plasma cells and CD138-19+ B cells progenitors obtained from newly diagnosed MM patients.
PATIENTS AND METHODS. The study included a cohort of 126 patients, homogenously treated with bortezomib-based regimens and ASCT, who were randomly included in a training set and a test set. For each patient, the CD138+ plasma cell fraction was isolated by immunomagnetic beads method; CD19+ B cells were isolated in 18 patients. Gene expression profiling (GEP) (HG U133 Plus 2.0 chip) and genomic analysis (SNP 6.0 chip) were performed on Affymetrix platform. dChip analysis software was used to perform GEP clustering. Expression data were analyzed by Ingenuity Pathway Analysis software and were validated by Western Blot assays. Copy number analysis was carried out using Nexus Copy Number software.
RESULTS. The expression of Hh pathway genes resulted deregulated in both CD138+ and CD19+ cells, as compared to their normal counterparts. By unsupervised hierarchical clustering, an Hh signature of 10 genes - SHH, IHH, DHH, SMO, PTCH1, PTCH2, SUFU, GLI1, GLI2 and GLI3 - was identified, and was able to significantly cluster patients in two subgroups: cluster 1 included 39 patients while 37 were included in cluster 2. Clustering robustness was validated in an independent cohort of 50 patients (test set), of whom 31 were assigned to cluster 1 and 19 to cluster 2. An overall significant activation of Hh pathway was shown in cluster 2, as compared to cluster 1. Of note, the Hh pathway was down regulated in CD19+ B cells obtained from patients included in cluster 2, while it was overexpressed in cluster 1 patients. Western blots on both cell fractions confirmed this opposite Hh genes behavior.
Peculiar genomic and transcriptomic profiles characterized patients included in clusters 1 and 2: indeed, a higher genomic instability (e.g. higher frequencies of both t(4;14) and del(17p)) was demonstrated in CD138+ plasma cells from cluster 2 patients and, at least 5 known tumor suppressor genes, such as RB1, BRCA2, PDX1, FOXO1 and TP53 were included in deleted regions. Conversely, cluster 1 patients were mainly characterized by hyperdiploid karyotypes. The more aggressive phenotype of cluster 2 patients was confirmed by an overall deregulation of cell adhesion processes (CD44, LIMS1, COL4A2, CTGF, COL1A1, FN1), increased proliferation (MYCBP, IL22, SDPR, SOX2, SOX6) and impaired DNA repair mechanisms (SP1, SMARCD3, FOXA3).
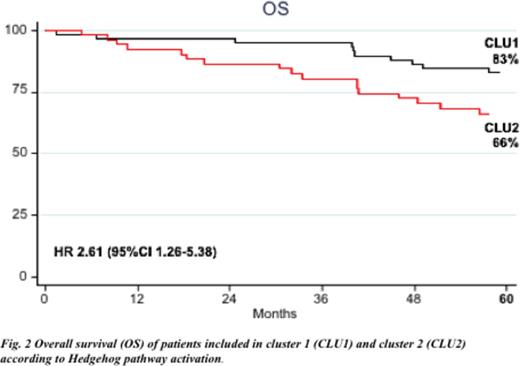
Hh pathway activation significantly influenced patientsÕ outcome, since those included in cluster 2 had a shorter PFS and OS compared to cluster 1. In fact, the 5-year PFS estimates were 31% vs 56% (p=0.0062), whereas the OS probabilities were 66% and 83%, respectively (p=0.0071) (Fig.1,2). Of note, both hazard ratios for PFS and OS were doubled in patients included in cluster 2, as compared to patients included in cluster 1. Finally, multivariate analyses confirmed that being included in cluster 2 was an independent prognostic factor for both PFS and OS, along with del(17p) and ISS 3 (Tab. 1).
CONCLUSION. Sorts of Òying -yang Ó effect of Hh pathway between mature CD138+ plasma cells and immature CD138-CD19+ MPCs could be hypothesized, where two alternate Hh-driven subtypes of MM at diagnosis correlated well with patientsÕ outcomes. Stratification of patients according to their molecular background might help the fine-tuning of future clinical studies.
Supported by Regione-Universita 2010-12 (L. Bolondi), FP7 NGS-PTL project.
Zamagni:Celgene Corporation: Honoraria, Speakers Bureau; Janssen Pharmaceuticals: Honoraria, Speakers Bureau; Amgen: Honoraria, Speakers Bureau. Martinelli:AMGEN: Consultancy; BMS: Consultancy, Speakers Bureau; Ariad: Consultancy; Novartis: Consultancy, Speakers Bureau; MSD: Consultancy; Pfizer: Consultancy; ROCHE: Consultancy. Cavo:Janssen-Cilag, Celgene, Amgen, BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal