Abstract
Introduction: We reported that microRNA-155 (miR-155) expression is upregulated in donor T cells during aGVHD and mice receiving miR-155 knock-out (KO) donor splenocytes do not exhibit lethal GVHD and have improved survival as compared to mice receiving wild type (WT) splenocytes.1 While we showed that miR-155 does not affect the allo-reactive proliferative potential of T cells, a significant decrease in the expression of the homing receptors CCR5, CXCR4, and S1P1 was found on miR-155-KO T cells, suggesting that the loss of miR-155 could impair the migration of donor T cells to aGVHD target organs resulting in less lethality. Here, we further investigate the impact of miR-155 expression in T cell migration.
Materials and Methods: Lethally irradiated BALB/c or B6D2F1 recipients were infused with T cell depleted WT bone marrow (BM) cells (5x10^6) and GFP expressing miR-155 KO or GFP-B6 WT T cells (1x10^6). Recipients were sacrificed at day 7, 14 and 21 post-transplant, organs harvested and donor T cell infiltration evaluated via confocal microscopy. Transwell migration assays towards CCR5 ligands macrophage inflammatory protein-1a (MIP-1a) (100ng/mL) and RANTES (100ng/mL) was performed utilizing WT or miR-155-KO T cells activated using irradiated BALB/c splenocytes as allogeneic stimulators at a stimulator: responder ratio of 1:5. Lower chambers with medium only served as a control for spontaneous migration. CCR5 ligand-dependent migration was calculated according to the formula: Migration Index (MI) = number of cells CCR5 ligands / number of cells medium only.
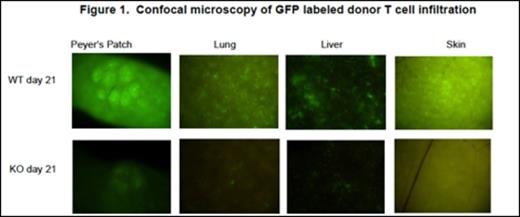
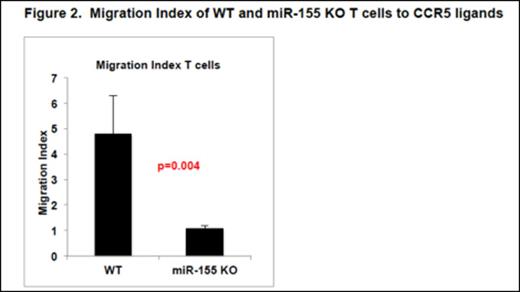
Results: On days 7, 14 and 21 post transplant, recipient mice were sacrificed, and tissues harvested in order to study the kinetics of miR-155 KO T cell migration following allogeneic hematopoietic stem cell transplant. There was a dramatic decrease in T cell infiltration of peripheral organs (PeyerÕs patches, liver, lung and skin) in recipients of miR-155-KO T cells as compared to WT T cells as evidenced by confocal microscopy of GFP labeled donor cells, Figure 1. We reasoned that these effects could be due to the modulation of CCR5 and other chemokine receptors by miR-155. There was a significant decrease in CCR5 mRNA and protein expression in miR-155-KO versus WT donor T cells obtained from recipient mice at the time of aGVHD. To demonstrate the functional significance of decreased CCR5 expression in miR-155 KO donor T cells, we performed in vitro transwell migration assays to CCR5 ligands RANTES and MIP-1a. To our knowledge, we are the first to show that allo-activated miR-155 KO T cells show significantly reduced migration towards CCR5 ligands, as demonstrated by the average MI of 1.08, when compared to the average MI of WT T cells of 4.79, p=0.004, Figure 2. There were lower percentages of CCR5 positive T cells and decreased mean fluorescent intensity in the miR-155 KO T cells after allogeneic stimulation when compared to WT T cells, both in the CD4+ and CD8+ populations, confirming lower CCR5 expression in miR-155 KO T cells after in vitro allogeneic stimulation.
To further elucidate the mechanism of miR-155 mediated modulation of CCR5 expression, we focused on long non-coding RNA (lncRNA) LincR-Ccr2-5′AS located in the vicinity of several chemokine receptor encoding genes including CCR1, CCR2 and CCR5, known to be important for migration of Th2 cells. We found that LincR-Ccr2-5′AS has 3 potential miR-155 binding sites and so set out to determine if miR-155 negatively regulates the expression of this lncRNA, thereby influencing chemokine receptor expression as well as T cell migration. We isolated T cells from B6D2F1 recipients 21 days post-transplant, and showed a significant decrease in CCR5 mRNA expression in miR-155 KO versus WT donor T cells but no significant difference in the levels of LincR-Ccr2-5′AS. However, this result does not exclude the possibility that miR-155 might influence the activity rather than the levels of LincR-Ccr2-5′AS, which we hope to determine in future experiments.
Conclusion: Our data suggest that miR-155 may exert its modulating effects in aGVHD by affecting T cell migration. Experiments are currently underway to determine the role of miR-155 in modulating T cell migration through other chemokine receptors such as CXCR4, as well as S1P1 and ATP receptor P2X7R.
Reference
1. Ranganathan P, Heaphy CE, Costinean S, et al. Regulation of acute graft-versus-host disease by microRNA-155. Blood. 2012 May 17;119(20):4786-97.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal