Abstract
Introduction - Allogeneic hematopoietic cell transplantation (HCT) is the only curative treatment for patients with myelofibrosis (MF). MF is stratified into various risk groups based on Dynamic International Prognostic scoring system (DIPSS plus), which determines the eventual prognosis of the disease at any time. Previous studies and expert opinion indicate that for patients with Intermediate-2 risk (INT-2) and High risk (HR) disease, HCT is a reasonable option. How applicable is this to all patients with MF and what are the barriers to doing a transplant are not known. We therefore reviewed medical records of all patients who were referred for HCT. The main purpose of this study was to determine the proportion of patients who underwent transplantation as well as to ascertain the major reasons why patients referred for transplantation did not receive it despite its reported benefit.
Methods- This was a retrospective, single institution, observational study. We analyzed patients referred for HCT with a diagnosis of MF. One hundred and ninety-eight consecutive patients with a preliminary diagnosis of MF were seen at the stem cell transplantation and cellular therapy (SCTCT) clinic of MD Anderson cancer center (MDACC) from 1/1/2004 to 12/31/2012. Out of the 198 patients, 26 had a diagnosis other than MF and hence were excluded. We stratified the remaining patients according to their DIPSS plus score at the initial consult and also traced their progression. For the non-transplanted patient with HR and INT-2 DIPSS plus scores, the major reason for deferring transplant was retrieved from the chart.
Results & Discussion- Out of 172 patients seen in the stem cell transplant clinic with MF, 70(41%) underwent transplantation and 102(59%) did not receive HCT. Of the 102 patients who did not undergo SCT, 72(70%) had INT-2 or HR disease at the initial consultation (transplant eligible). Of the remaining 30 patients with low risk or intermediate-1 risk disease, 7(23%) patients eventually progressed to INT-2 or HR disease and became transplant eligible. The median time from MF diagnosis to consultation for non-transplanted patients was 331days (11 months) (Range-0-8675).
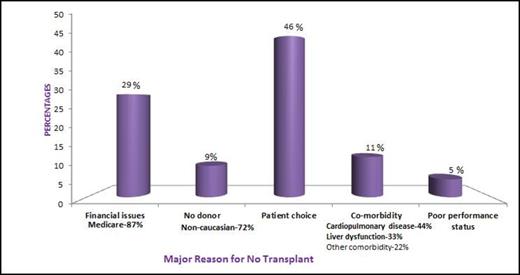
For patients with INT-2 and HR disease (79/102), the major reasons for not receiving a transplant (Figure) are patient choice (36/79; 46%), financial issues (23/79; 29%), comorbidities (9/79; 11%), lack of donor (7/79; 9%) and poor performance status (4/79; 5%). Patient choice of not pursuing transplant is understandable because there was limited data on efficacy of HCT for MF in early years. The most common insurance provider not covering transplantation was Medicare (20/23; 87%). The co-morbidities that precluded HCT were cardiopulmonary disease (4/9; 44%), liver dysfunction due to advanced disease (3/9; 33%) and other comorbidities (2/9; 22%). Of note 5/7 (72%) patients who were not transplanted due to lack of appropriate donor were non-Caucasian patients.
Conclusion- Only 41% of patients referred for transplant with MF receive HCT. The major barriers to wider application and usage of HCT for MF were patient choice and lack of coverage by Medicare. Patient education, coverage by Medicare, use of alternative donors, and earlier transplant referrals can further increase the accessibility of transplantation and improve outcomes of patients with MF.
Alousi:Therakos, Inc: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal