Abstract
Background: Pain, the hallmark complication of sickle cell disease (SCD), is largely managed with opioid analgesics in the United States (1, 2). There is a common perception that SCD patients tend to use high dose of opioids chronically (3, 4), but comprehensive data regarding the long-term use of opioids in this patient population is lacking.
Methods: A cohort of 359 adults (age ≥ 18 years old) with the diagnosis of SCD followed at University of Illinois Hospital in FY 2010-2013 was enrolled in a prospective natural history study. An outpatient clinic visit with comprehensive laboratory closest to the enrollment date was selected as the focal point of this report. A total of 140 patients had consistent outpatient follow-up defined as ³4 visits between 6 months prior to and 6 months after this clinic visit (the study period). Pain medication prescribing records, number of hospital admissions, and other clinical variables during the study period were collected and evaluated with descriptive statistics and Spearman correlation.
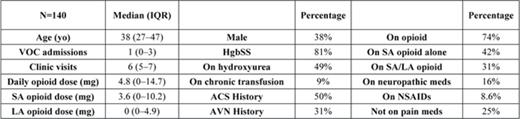
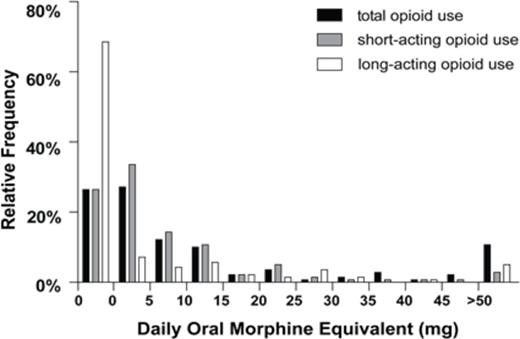
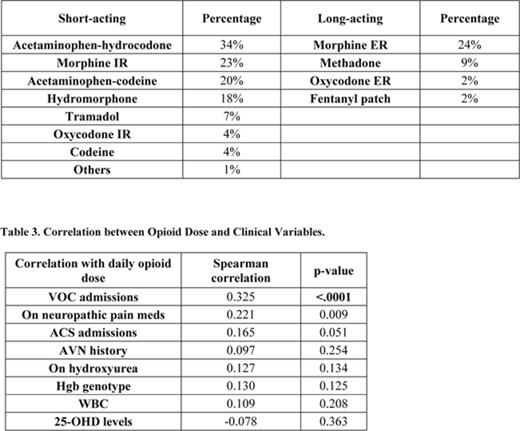
Results: Among the 140 patients analyzed, 74% took short-acting opioid medications and 31% took long-acting opioid medications (Table 1). The median daily opioid dose was 4.8 mg oral morphine equivalents (OME) with an interquartile range (IQR) of 0 to 14.7 mg. Sixty-six percent of patients used less than 10 mg OME daily whereas 11% used more than 50 mg OME daily (Figure 1). Among the short-acting opioids, acetaminophen-hydrocodone was the most commonly used medication (34% of patients) followed by immediate-release morphine (23%) and acetaminophen-codeine (20%) (Table 2). Extended-release morphine was used by 24% of the patients. Twelve patients (8.6%) were prescribed with nonsteroidal anti-inflammatory drugs (NSAIDs), and 16% used medications treating neuropathic pain. The Spearman correlation test with Bonferroni correction showed that the dose of opioid usage was significantly associated with the number of hospital admissions due to vaso-occlusive crisis (VOC) (p<0.0001) (Table 3). Hydroxyurea use, hemoglobin genotype, history of avascular necrosis (AVN) and 25-OHD levels did not correlate with opioid dose.
Summary: The doses and types of opioid medications used by adult SCD patients vary widely. The majority of patients use a relatively low dose (<10 mg OME daily). The dose of chronic opioid use has a strong correlation with the frequency of hospital admissions due to VOC, demonstrating the necessity of finding an alternative pain management approach in treating sickle cell pain.
1. L. R. Solomon, J Natl Med Assoc102, 1025 (Nov, 2010).
2. P. Tanabe, Z. Martinovich, B. Buckley, A. Schmelzer, J. A. Paice, J Emerg Nurs41, 227 (May, 2015).
3. W. T. Zempsky, JAMA302, 2479 (Dec 9, 2009).
4. B. S. Shapiro, L. J. Benjamin, R. Payne, G. Heidrich, J Pain Symptom Manage14, 168 (Sep, 1997).
The relative frequency = the number of patients taking certain dose of opioids/total number of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal