Abstract
Introduction -Washed red blood cell (RBC) and platelet transfusions have been a valuable therapeutic option for patients with repeated or severe allergic or febrile reactions. Recent data from randomized and observational clinical trials demonstrate that washed transfusions reduce inflammatory and immunologic complications, including recurrence of acute leukemia, death after coronary surgery, elevations of IL-6 and C-reactive protein after pediatric cardiac surgery, and transfusion related acute lung injury and transfusion associated cardiac overload. However, washing of RBCs may not be completely benign. Increased hemolysis may occur in vitro. Washing of RBCs stored for longer periods (>28 days) is associated with increased morbidity in pediatric cardiac surgery patients receiving massive transfusions of older RBCs. Current washing techniques and dilution of RBCs for transfusion employ 0.9% normal saline (NS) which is both hypertonic and acidic. We evaluated whether use of a more physiologic solution, Plasma-Lyte, causes less damage to RBCs than use of NS.
Methods -We employed RBC units (n=15) collected for, but not suitable for clinical transfusion. Median storage age was 19 days (range 10-39 days). Each donor unit (11 AS-1, 3 AS-3 and 1 CPD-A1) was split in two using aseptic technique, and washed with either a liter of NS or Plasma-Lyte employing a standard clinical protocol on a Terumo 2991. Each half was resuspended in 20 ml of washing solution. Aliquots (12 ml) were removed prior to and immediately after washing, and after 24, 48 and 72 hours of storage at 1-6¡ C. These aliquots were immediately centrifuged (15 min at 4,300 x g) and the supernatant stored at -80¡ C. Hemoglobin and heme in the supernatant were quantitated using QuantiChrom kits. All comparisons were by Wilcoxon matched pairs non-parametric tests.
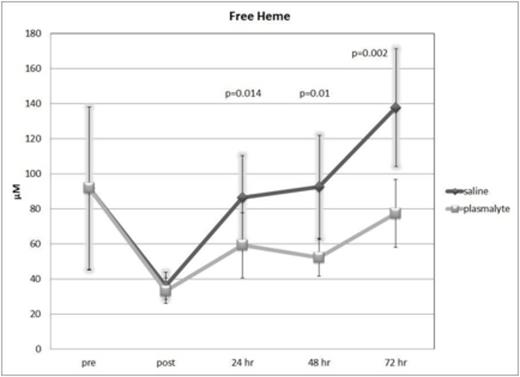
Results -Supernatants immediately after washing had similar mean free hemoglobin (pre = 160 mg/dl ± 80 [SEM]; post = 66 ± 12 for NS and 58 ± 10 for Plasma-Lyte) and heme (pre = 92 µM ± 46; post = 36 ± 8 for NS and 33 ± 7 for Plasma-Lyte ). However, by 24 hours of storage after washing (the current limit for clinical use), supernatant heme and hemoglobin were significantly greater by about 50% in RBCs stored in NS (87 µM ± 22 and 151 mg/dl ± 36) as compared to Plasma-Lyte (59 µM ± 21 and 108 mg/dl ± 36; p = 0.014 and 0.02). These changes accelerated during subsequent storage (see figure for heme levels-differences in hemoglobin were comparable). Prolonged storage after NS washing predisposed to greater hemolysis than did Plasma-Lyte washing. Supernatant heme levels at 72 hours post washing increased from early (10-18 days; n=5) to late (31-39 days; n=5) storage by a mean of 61% in Plasma-Lyte washed RBCs (p=0.26) compared with 200% in NS washed RBCs (p=0.016)
Conclusions -RBCs stored for 10-39 days and then washed with Plasma-Lyte experience strikingly less hemolysis. Whether such differences would occur in vivo is not known, and the clinical implications are yet to be determined. Circulating free heme and hemoglobin levels have been associated with thrombosis in animal models, transfused patients and patients with sickle cell disease. NS, as opposed to Plasma-Lyte, has been linked to increased renal injury and mortality in animal models and patients. We speculate that hemolysis may be a contributing cause. Our results indicate that RBC washing with Plasma-Lyte is a superior approach and potentially safer than NS. These findings also suggest the hypothesis for further investigation of whether NS is truly a suitable diluent for RBC transfusion, and whether NS is the safest choice when crystalloid is indicated for volume replacement or apheresis. Plasma-Lyte washing might also facilitate increasing the storage period of washed RBCs.
Off Label Use: See Dr. Blumberg's disclosure. Blumberg:Biomet: Consultancy; Terumo: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal