Abstract
Background: Hematopoietic stem cell transplantation (HSCT) is the only curative treatment for patients with thalassemia major. Majority of the patients undergoing transplants in India belongs to advanced Pesaro risk stratification and 2013 data from India using treosulfan based conditioning for matched related donor transplants (MRD) has showed an event free survival of 78.8 ± 6.0 at 3 years (Mathews et al. Plos One 2013). Advanced age and risk stratification is a deterrent in proceeding with matched unrelated donor (MUD) transplant in India. Since only 25-30 % of patients are likely to get a MRD, MUD transplant is a feasible option in the background of limited life expectancy in patients with thalassemia major. However, there is no data comparing MRD and matched unrelated donor (MUD) transplants from India.
Method: This is a retrospective analysis to compare the outcomes between MRD and MUD transplants from a single institution. Events were defined as primary graft failure, graft rejection leading to recurrence of transfusion dependence or death.
Results: A total of 123 patients with thalassemia major underwent MUD search in DKMS and DATRI registries. Fifteen (12%) and 13 (10%) patients found 10/10 HLA identical donors respectively and 4 (3%) of them had matches in both the registries. Very few patients underwent NMDP search due to cost constraints.
Among the 36 patients who underwent stem cell transplantation, MRD group had 27 patients and MUD group has 9 patients. Base line characteristics of age, sex and Pesaro risk stratification were matched. (Table: 1) Majority of patients belonged to high risk category in both the groups. The conditioning regimens used in both the groups were thiotepa, fludarabine, and treosulfan (TreoFluT). All the MRD non-sibling transplants and MUD transplants also received antithymocyte globulin (ATG) as part of the conditioning regimen. All patients received HLA identical (10/10) grafts. In the MRD group, the stem cell source was 24 (89%), 2 (7%) and 1 (4%) from sibling, parent and 1st cousin respectively. The MUD grafts were procured from 3 different registries DKMS (German) 5 (56%), NMDP (US) 2 (22%) and DATRI (Indian) 2 (22%). Cyclosporine and short course methotrexate were used as Graft versus host disease (GVHD) prophylaxis in all the patients
Multiple challenges are involved in the availability and procurement of donor grafts from different registries. A special DCGI (Drug controller General of India) approval needs to be taken for every graft source procured from overseas. The estimated average cost of MRD transplant is 24000 US$ and MUD transplant is 48000 US$ for DKMS and DATRI grafts and 78000 US$ for NMDP grafts. Inspite of lower costs than the western countries, affordability is a major concern even if matched donors are available.
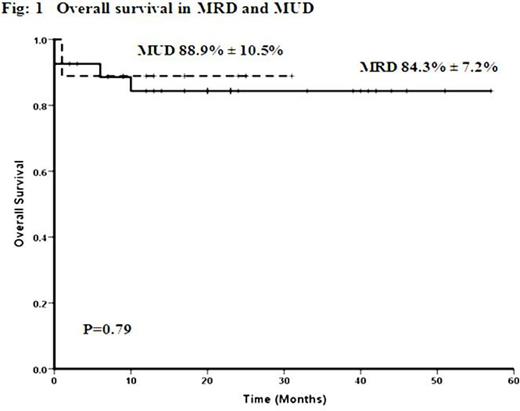
Overall survival at 1 year in MRD and MUD groups was 84.3 ± 7.2% and 88.9 ± 10.5% at a median follow up of 20 (0-57) months and 13 (1-31) months respectively (p= 0.799) (Fig:1). The thalassemia free survival at 1 year was 84.3 ± 7.2% and 77.8 ± 13.9% with a median follow up of 20 (0-57) and 12 (1-31) months respectively (p= 0.732). (Fig: 2).
Conclusion: Although the incidence of acute GVHD and chronic GVHD incidence are higher in the MUD transplant group, TreoFluT based conditioning for allogeneic stem cell transplantation with both matched related and unrelated donor graft source is a feasible option in beta thalassemia major patients even in high risk category from developing countries.
Patient demographics and transplant characteristics
| . | MRD (n= 27) n(%) Median(range) Mean ± SD . | MUD n=9 n(%) Median(range) Mean ± SD . | P-value . |
|---|---|---|---|
| Age (yrs) | 10 (2-18) | 9 (2-18) | 0.502 |
| Sex: Male | 19 (70) | 6 (66) | 0.835 |
| Class I | 1 (4) | 2 (22) | 0.135 |
| Class II | 6 (22) | 3 (33) | |
| Class III | 20 (74) | 4 (44) | |
| Class III Vellore high risk | 11 (55) | 3 (75) | 0.693 |
| Stem cell source | |||
| PBSC BM BM + CB BM + PBSC + CB | 23 (85) 2 (7) 1 (4) 1 (4) | 7 (78) 2 (22) 0 0 | 0.599 |
| Cell dose | |||
| MNC/TNC x 108/Kg CD34 x 106/Kg | 8.04 (3.49 -14.6) 5.91 (0.23 -27.75) | 7.2 (2.83 -10.47) 8.47 (0.49 -21.6) | 0.782 0.381 |
| Acute GVHD | 6 (22) | 6 (66) | 0.014 |
| Grades I and II | 5 (19) | 4 (44) | 0.505 |
| Grades III and IV | 1 (4) | 2 (22) | |
| Classic acute GVHD | 5 (18) | 3 (33) | 0.287 |
| Persistent | 0 | 0 | |
| Recurrent | 0 | 3 (33) | |
| Late onset | 1 (4) | 0 | |
| Chronic GVHD | 6 (22) | 6 (67) | 0.014 |
| Classic Chronic GVH | 5 (18) | 3 (33) | 0.545 |
| Overlap syndrome | 1 (4) | 3 (33) | |
| . | MRD (n= 27) n(%) Median(range) Mean ± SD . | MUD n=9 n(%) Median(range) Mean ± SD . | P-value . |
|---|---|---|---|
| Age (yrs) | 10 (2-18) | 9 (2-18) | 0.502 |
| Sex: Male | 19 (70) | 6 (66) | 0.835 |
| Class I | 1 (4) | 2 (22) | 0.135 |
| Class II | 6 (22) | 3 (33) | |
| Class III | 20 (74) | 4 (44) | |
| Class III Vellore high risk | 11 (55) | 3 (75) | 0.693 |
| Stem cell source | |||
| PBSC BM BM + CB BM + PBSC + CB | 23 (85) 2 (7) 1 (4) 1 (4) | 7 (78) 2 (22) 0 0 | 0.599 |
| Cell dose | |||
| MNC/TNC x 108/Kg CD34 x 106/Kg | 8.04 (3.49 -14.6) 5.91 (0.23 -27.75) | 7.2 (2.83 -10.47) 8.47 (0.49 -21.6) | 0.782 0.381 |
| Acute GVHD | 6 (22) | 6 (66) | 0.014 |
| Grades I and II | 5 (19) | 4 (44) | 0.505 |
| Grades III and IV | 1 (4) | 2 (22) | |
| Classic acute GVHD | 5 (18) | 3 (33) | 0.287 |
| Persistent | 0 | 0 | |
| Recurrent | 0 | 3 (33) | |
| Late onset | 1 (4) | 0 | |
| Chronic GVHD | 6 (22) | 6 (67) | 0.014 |
| Classic Chronic GVH | 5 (18) | 3 (33) | 0.545 |
| Overlap syndrome | 1 (4) | 3 (33) | |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal