Abstract
Introduction
Haploidentical family donors are becoming an effective alternative for patients in need of an hematopoietic stem cell transplantation (HSCT) but lacking an HLA-matched donor. However, to prevent graft-versus-host disease (GVHD), intensive in-vivo or ex-vivo T-cell depletion is often utilised, resulting in slow immune reconstitution, frequent and often lethal infectious complications and/or high relapse rates, thus decreasing overall survival.
To overcome these limitations, we have developed a strategy that allows additional donor lymphocytes to be infused post-HSCT without the risk of inducing severe GVHD and maintaining the ability to react against infections and leukemic cells.
Patients and Methods
In this open-label, multi-centre phase 2 clinical trial (CR-AIR-007; NCT01794299), 23 patients with high-risk AML or ALL were enrolled. Patients underwent myeloablative conditioning and were given a CD34+ selected stem cell graft from a haploidentical family donor. In addition, donor lymphocytes from the same donor were processed using a selective photodepletion technology, creating a donor lymphocyte product depleted of alloreactive T-cells (ATIR101). ATIR101 was to be given to patients at 28-32 days post-HSCT at a fixed dose of 2x106 CD3+ cells/kg. No post-transplant GVHD prophylaxis was administered.
The primary endpoint of the study is transplant-related mortality at 6 months post-HSCT. Patients are followed to determine disease-free and overall survival.
Patients undergoing a similar T-cell depleted haploidentical HSCT without ATIR infusion (CR-AIR-006; NCT02188290) were used as controls. Most centers providing the historic control data also participate in this phase 2 trial with ATIR101.
Results
Twenty-three patients, median age of 41 years (range 21 - 64), have been enrolled into this study. Seventeen patients, 7 male and 10 female, had AML, 12 in CR1 and 5 in CR2 at the time of HSCT. Six patients, 5 male and 1 female, had ALL, 4 in CR1 and 2 in CR2 at the time of HSCT.
Conditioning regimen consisted of a] TBI (1200 cGy; n=10) or b] melphalan (120 mg/m2; n=12), along with thiotepa (10 mg/kg), fludarabine (30 mg/m2 x 5d) and ATG (2.5mg/kg x 4d). No patient experienced graft rejection, with neutrophil and platelet engraftment achieved at a median of 11 and 12 days, respectively (range 8-18, range 9-35). 21 patients to date received ATIR101, at a fixed dose of 2x106 CD3+ cells/kg at a median of 28 days (range: 28-73 days) post-transplant. Median follow-up is 270 Days post-HSCT.
No patient developed grade III-IV acute GVHD. Two cases of grade II acute GVHD were reported thus far. The onset of these two acute GVHD cases was delayed, at day 173 and day 247 post-HSCT, 145 and 219 post ATIR respectively.
No patient died within the first 100 days post-HSCT. There are 3 deaths as a result of transplant related mortality within 6 months post-HSCT (primary endpoint).
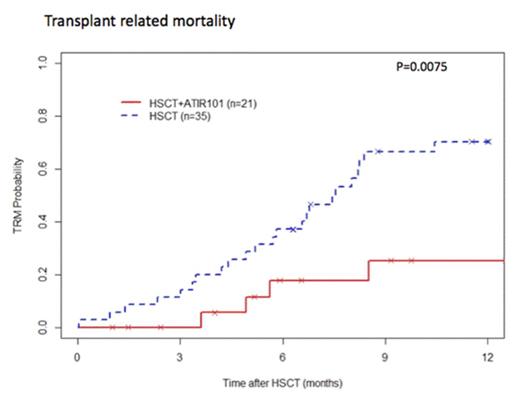
When compared to the matched historic control group (N=35), TRM was significantly lower in patients given ATIR101 after a T-cell depleted haplotransplant with a 6-month TRM for HSCT + ATIR101 of 17% versus 34% for HSCT only (Figure 1a).
Figure 1a: Kaplan Meier of Transplant related mortality: HSCT + ATIR101 vs HSCT alone (p=0.0075), data as per 3 August 2015.
Thus far, in CR-AIR-007 study, only one patient experienced a relapse, which occurred at 90 days post-HSCT and resulted in death of the patient on day 122.
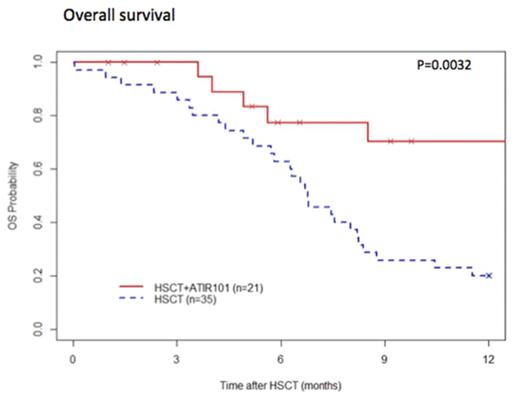
The overall survival of patients given ATIR101 is significantly improved, compared to the control group, with a 1-year survival of 67% in the HSCT + ATIR101 group and 20% in the control group (Figure 1b).
Figure 1b: Kaplan Meier of Overall Survival: HSCT + ATIR101 vs HSCT alone (p=0.0032), data as per 3 August 2015.
Conclusions
Addition of ATIR101 to a T-cell depleted haploidentical HSCT protocol significantly improves transplantation outcome, with reduced TRM and improved OS. Specifically, no patient died during the first 100 days post-HSCT. Administration of ATIR101 at the dose of 2x106 cells/kg does not induce severe GVHD, confirming the efficacy of alloreactive T-cell elimination from the donor lymphocyte infusion. We attribute the reduced TRM (mainly infections in the control group) to the additive immunological protection afforded by ATIR101. Moreover, the low number of relapses observed thus far is most encouraging and supports the preservation within ATIR101 of T-cells able to recognize leukemic antigens.
Roy:Kiadis Pharma: Consultancy, Research Funding; Novartis: Honoraria. Rudiger:Kiadis Pharma: Employment. Velthuis:Kiadis Pharma: Employment. Reitsma:Kiadis Pharma: Employment. Gerez:Kiadis Pharma: Employment. Rovers:Kiadis Pharma: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal