Abstract
Introduction: Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is an aggressive hematologic malignancy derived from plasmacytoid dendritic cells (pDC). Today, no therapeutic consensus exists and only allogeneic hematopoietic cell transplantation provides a durable remission. BPDCN cells express high levels of the IL-3 receptor alpha chain (CD123) and exhibit an increased survival and growth in response to IL-3 (Chaperot et al. 2001). Recently, aberrant NF-κB activation has been reported in BPDCN (Sapienza et al. 2014), and we identified that liver X receptor (LXR) stimulation inhibits NF-κB activation in non-leukemic pDC. LXR represent nuclear receptors promoting cholesterol efflux via the ATP binding cassette A1 and G1 (ABCA1 and ABCG1, respectively) transporters and lipid acceptors, such as apolipoprotein A1 (ApoA1). This process has been shown to repress IL-3-induced proliferation of murine hematopoietic stem cells (Yvan-Charvet et al. 2010). The aim of this study was to investigate LXR activation in BPDCN, and determine whether LXR agonists possess therapeutic effects.
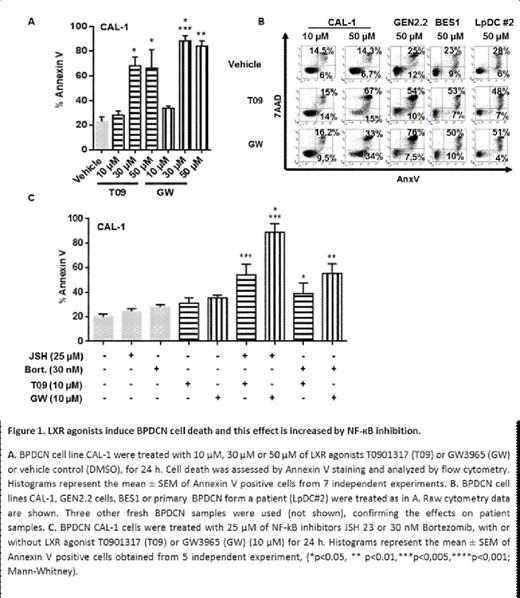
Material and Methods: Cells from 13 BPDCN, 22 undifferentiated AML, 23 ALL patients and 4 normal pDC were evaluated for expression of LXR or cholesterol exchange related genes (lxra, lxrb, abca1, abcg1, apoe, srebp1c, ldlr, vldlr), plus nfkb1 gene by Affymetrix mRNA microarray. BPDCN cells (2 established cell lines [GEN2.2, CAL-1], a primary cell line [BES1] and 5 fresh BPDCN samples) were treated with two LXR agonists (T0901317 [T09] or GW3965 [GW] at 1 µM, 10 µM or 50 µM), NF-κB inhibitors (JSH 23, or Bortezomib [Bort]) and the cholesterol acceptor ApoA1 (10 µg/mL). Gene expression (abca1, abcg1, nfkb1, bcl2, bax and bak1) was assessed by qRT-PCR. Cell death was assessed by Annexin V/7AAD staining (flow cytometry) and caspase activation (Western blot). CAL-1 cell proliferation was assessed by dye dilution (cytometry). Cholesterol efflux was measured directly by H3 cholesterol efflux from cells and indirectly by membrane ABCA1 expression (confocal microscopy). NF-κB and IL-3 signaling pathway activation was explored by protein phosphorylation (phospho-RelA and phospho-STAT5, respectively; [confocal microscopy and Western blot]). A BPDCN xenograft model was used to evaluate LXR agonist effect in-vivo with blast cell infiltration attested by human CD45/CD123/BDCA4 staining (cytometry).
Results: BPDCN cells showed a unique transcriptomic signature with LXR-related gene downregulation. LXR agonist treatment for 24h restored LXR target gene expression, including abca1 and abcg1, and induced a significant concentration-dependent killing (Fig. 1). Moreover, caspase 8 and 9 cleavage associated with bcl2 downregulation and bax and bak1 upregulation (0.78, 8 and 12.2 fold mRNA levels, respectively, for GW 50 µM, 6h, n=3) were observed. At a lower non cytotoxic concentration (10 µM), GW treatment inhibited cell proliferation (-25%, p<0.05, n=7) that was reinforced by addition of ApoA1 (-35%, n=2). This suggests a link with cholesterol efflux supported by induction of ABCA1 expression at BPDCN membrane and increase of H3 cholesterol efflux in response to LXR agonists. LXR agonists inhibited IL-3-induced STAT5 phosphorylation and NF-κB signaling pathway at transcriptional (nfkb1, 0.25 fold mRNA level, p<0.05, n=3 fresh BPDCN samples) and RelA phosphorylation levels. This suggests additional mechanisms by which LXR activation affects BPDCN. NF-kB inhibitor treatment (JSH23, 25 µM, 24h) reduced BPDCN survival (-35%, n=3) and proliferation (-20%, p<0.05, n=3). A synergic effect of NF-κB inhibitors (JSH23 25 µM or Bort 30 nM) and LXR agonists (GW or T09, 10 µM), was observed on cell death and inhibition of proliferation (Fig. 1). The in-vivo study revealed a reduced CAL-1 infiltration in the spleen and bone marrow of T09-treated mice (1.2 mg/2 days for 14 days) compared with control mice (62% vs. 33% and 17% vs. 9%, respectively). Effects of LXR plus NF-κB inhibitor treatment in vivo are under investigation.
Conclusion: BPDCN exhibit a specific transcriptomic signature with LXR-related gene downregulation. LXR stimulation of BPDCN restores LXR-related gene expression and inhibits survival and proliferation. This may occur via several mechanisms: inhibition of IL-3 and NF-κB signaling, and/or increased cholesterol efflux. A cytotoxic or cytostatic effect was confirmed in-vivo by reduced BPDCN infiltration.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal