Abstract
Introduction: Black patients with acute myeloid leukemia (AML) have inferior overall survival relative to White patients. Few studies have evaluated differences in induction mortality and none has assessed the contribution of severity of illness at presentation to the disparity in survival. Our primary objectives were to compare induction mortality and acuity of presentation among Black relative to White patients and to assess whether any disparity in induction mortality is the consequence of differences in presentation acuity. In addition, we explored the interaction between Black race and public insurance on induction mortality with use of single referent models.
Methods: Using a retrospective cohort of children (ages 0 to 18 years) from 2004 to 2014 with new-onset AML diagnosed and treated at free-standing pediatric hospitals who contribute inpatient information to the Pediatric Health Information System administrative database (PHIS), we evaluated inpatient mortality over two courses of standard induction chemotherapy. We examined race (Black versus White) as the primary exposure and insurance was considered with race using a common reference group. We also considered Intensive Care Unit (ICU)-level resource use during the first 72 hours following the initial AML admission as a surrogate for acuity at presentation and a potential mediator of the association between race and induction mortality.
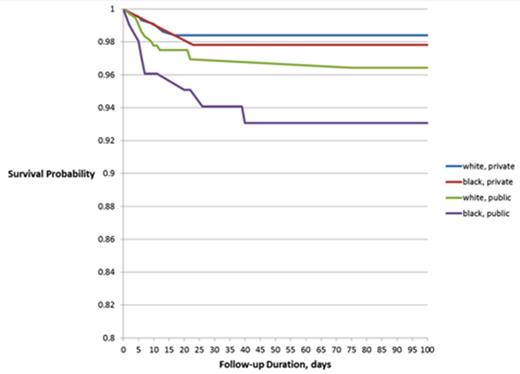
Results: 1,122 patients (183 Black, 939 White) with AML who received standard induction chemotherapy were included. Induction mortality for Blacks was substantially higher than for Whites (cHR= 2.31, 95% CI: 1.01, 5.42). Blacks also had a significantly higher risk of requiring any ICU-level care within the first 72 hours after initial presentation compared with Whites (cHR= 1.52, 95% CI: 1.02, 2.24).The association between race and induction mortality was attenuated following adjustment for ICU-level care within the initial 72 hours after admission, (aHR=1.42, 95% CI: 0.67, 2.99). Publicly insured patients experienced greater induction mortality than privately insured patients regardless of race. Induction mortality rates for Black and White patients were more similar among the privately insured and were increasingly disparate among the publicly insured.
Conclusion: Our findings suggest that Black patients with AML present with more acute illness at initial diagnosis, accounting for up to 63% of the relative excess induction mortality. Identifying factors impacting acuity of illness at presentation and associated with public insurance may help to identify opportunities for intervention and thus narrow the current racial disparities in pediatric AML survival.
Inpatient Induction Mortality and ICU level Care by Race
| Outcome, Follow-up Period . | Overall (N=1122) n (%) . | Black (n=183) n (%) . | White (n=939) n (%) . | cHR (95% CI) . | aHRa (95% CI) . |
|---|---|---|---|---|---|
| Induction Death | 27 (2.4%) | 8 (4.4%) | 19 (2.0%) | 2.31 (1.01, 5.42) | 1.42 (0.67, 2.99) |
| Any ICU Level Care in first 72 hrs | 135 (12.0%) | 31 (16.9%) | 104 (11.1%) | 1.52 (1.04, 2.24) | |
| ICU involving >1 system in first 72 hrs | 47 (4.2%) | 18 (9.8%) | 29 (3.1%) | 3.35 (1.84, 6.12) | |
| Any ICU Level Care in Induction | 237 (21.1%) | 48 (26.2%) | 189 (20.1%) | 1.30 (0.99, 1.71) | 1.09 (0.74, 1.61) |
| ICU involving >1 system in Induction | 99 (8.8%) | 22 (12.0%) | 77 (8.2%) | 1.42 (0.85, 2.38) | 0.92 (0.54, 1.57) |
| Outcome, Follow-up Period . | Overall (N=1122) n (%) . | Black (n=183) n (%) . | White (n=939) n (%) . | cHR (95% CI) . | aHRa (95% CI) . |
|---|---|---|---|---|---|
| Induction Death | 27 (2.4%) | 8 (4.4%) | 19 (2.0%) | 2.31 (1.01, 5.42) | 1.42 (0.67, 2.99) |
| Any ICU Level Care in first 72 hrs | 135 (12.0%) | 31 (16.9%) | 104 (11.1%) | 1.52 (1.04, 2.24) | |
| ICU involving >1 system in first 72 hrs | 47 (4.2%) | 18 (9.8%) | 29 (3.1%) | 3.35 (1.84, 6.12) | |
| Any ICU Level Care in Induction | 237 (21.1%) | 48 (26.2%) | 189 (20.1%) | 1.30 (0.99, 1.71) | 1.09 (0.74, 1.61) |
| ICU involving >1 system in Induction | 99 (8.8%) | 22 (12.0%) | 77 (8.2%) | 1.42 (0.85, 2.38) | 0.92 (0.54, 1.57) |
a adjusted for ICU acuity score within the first 72 hours of index admission
Independent and joint effects of Black race and public insurance on induction mortality
Independent and joint effects of Black race and public insurance on induction mortality
Wilkes:Alex's Lemonade Stand Foundation: Research Funding; Healthcare Research and Quality: Research Funding. Fisher:Merck: Research Funding; Pfizer: Research Funding. Epstein:Medicus Economics: Consultancy. Aplenc:Sigma Tau: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal