Key Points
Warfarin-induced venous gangrene in cancer affects limb with DVT and features platelet fall after stopping heparin and supratherapeutic INR.
Persisting thrombin generation occurs despite elevated INR, indicating severe PC depletion that occurs in parallel with reduced factor VII.
Abstract
Venous limb gangrene (VLG) can occur in cancer patients, but the clinical picture and pathogenesis remain uncertain. We identified 10 patients with metastatic cancer (7 pathologically proven) who developed severe venous limb ischemia (phlegmasia/VLG) after initiating treatment of deep-vein thrombosis (DVT); in 8 patients, cancer was not known or suspected at presentation. The patients exhibited a novel, clinically distinct syndrome: warfarin-associated supratherapeutic international normalized ratio (INR; median, 6.5) at onset of limb ischemia, rising platelet count during heparin anticoagulation, and platelet fall after stopping heparin. Despite supratherapeutic INRs, patient plasma contained markedly elevated thrombin-antithrombin (TAT) complex levels (indicating uncontrolled thrombin generation) and protein C (PC) depletion; this profile resembles the greatly elevated TAT/PC activity ratios reported in patients with warfarin-associated VLG complicating heparin-induced thrombocytopenia. Analyses of vitamin K–dependent factors in 6 cancer patients with available serial plasma samples showed that variations in the INR corresponded most closely with changes in factor VII, with a highly collinear relationship between VII and PC. We conclude that venous limb ischemia/gangrene is explained in some cancer patients by profoundly disturbed procoagulant-anticoagulant balance, whereby warfarin fails to block cancer-associated hypercoagulability while nonetheless contributing to severe PC depletion, manifest as a characteristic supratherapeutic INR caused by parallel severe factor VII depletion.
Introduction
Warfarin and other vitamin K antagonists impair synthesis of the vitamin K–dependent coagulation factors. The most common complication is bleeding, which results from reduction in the vitamin K–dependent procoagulant factors, prothrombin (factor II) and factors X, IX, and VII. Less often, warfarin causes microvascular thrombosis, a complication believed to result primarily from decreased levels of 1 or both of the vitamin K–dependent natural anticoagulants, protein C (PC) and protein S.1,2 The classic picture of “coumarin necrosis” involves dermal/subdermal tissues predominantly at nonacral sites (eg, breast, abdomen, thigh, calf, and forearms).1,2
Warfarin therapy has also been implicated in the pathogenesis of venous limb gangrene (VLG).2-5 Unlike classic skin necrosis, these patients exhibit acral (distal extremity) necrosis involving a limb affected by deep-vein thrombosis (DVT), with more extensive necrosis than skin alone. Patients have palpable or Doppler-identifiable arterial pulses, as the pathogenesis involves thrombosis of large veins and smaller venules/microcirculation. Warfarin-induced VLG is an important explanation for limb loss in patients with heparin-induced thrombocytopenia (HIT); in such patients, there is profoundly disturbed procoagulant-anticoagulant balance, with HIT-induced hypercoagulability (disseminated intravascular coagulation [DIC]), shown by markedly increased thrombin-antithrombin (TAT) complexes, and severe PC depletion.4 Affected patients characteristically have a supratherapeutic international normalized ratio (INR).4,5
There are also case reports of warfarin-induced VLG complicating metastatic cancer, usually adenocarcinoma.6-10 The clinical features and pathogenesis of this syndrome are obscure, although 2 reports7,8 provided laboratory data (increased TAT to PC activity ratio) suggesting a model of disturbed procoagulant-anticoagulant balance mimicking that seen in HIT/warfarin-induced venous limb ischemia. We now report 10 patients with cancer-associated severe venous limb ischemia/gangrene allowing us to characterize the clinical and laboratory picture. Our study provides further evidence that the pathogenesis of warfarin-associated venous limb ischemia in cancer resembles that seen in HIT. Moreover, patients exhibit a characteristic clinical picture, namely: (1) platelet count rise on heparin, and platelet count fall after stopping heparin (because of recurrent consumptive coagulopathy, ie, “cancer associated DIC”); (2) supratherapeutic INR secondary to warfarin; and (3) severe venous limb ischemia/gangrene in the limb affected by DVT. Interestingly, most patients were not known to have had cancer at development of limb ischemia, and all patients had metastatic disease when cancer was diagnosed.
Methods and patients
We identified 10 patients with severe venous limb ischemia or gangrene complicating cancer, using 2 approaches. First, from a list of 1134 patients from 2 hospitals affiliated with Hamilton Health Sciences (General Hospital, n = 875; McMaster Hospital, n = 259) who tested negative during a 10-year period in the serotonin-release assay (SRA) for the antibodies that cause HIT, we identified patients with admission diagnostic codes ranging from 140.0 to 199.1 (codes indicating a cancer diagnosis reported in the medical records). This approach identified 98 patients, for which the medical records were reviewed to determine occurrence of severe venous limb ischemia, either phlegmasia cerulea dolens (PCD; severe venous limb ischemia with threatening limb loss) or VLG (acral tissue necrosis, including amputation). This review resulted in 8 patients being identified with cancer-associated venous limb ischemia. Further, an additional 2 cases were identified by 1 investigator (T.E.W.) during his consultative practice after the study period ended. Thus, 10 patients with cancer-associated severe venous limb ischemia/gangrene were identified.
For the patient files reviewed, 2 hematologists (T.E.W., M.A.C.) reached consensus on the most likely explanation for thrombocytopenia (that led to HIT antibody testing) for each patient, within one of the following categories: (1) cancer-associated DIC; (2) postoperative hemodilution/consumption; (3) septicemia/multiorgan system failure; (4) nonseptic shock (eg, cardiogenic shock); (5) leukoerythroblastosis/marrow replacement; (6) postthrombolysis; (7) (non-HIT) drug-induced immune thrombocytopenia; (8) hematophagocytosis syndrome; (9) isolated thrombosis (despite absence of thrombocytopenia); (10) nonimmune heparin-associated thrombocytopenia (transient otherwise unexplained thrombocytopenia beginning within 2 days of heparin treatment); (11) chemotherapy or radiation therapy; (12) intravascular/intracardiac tumor; (13) tumor-associated thrombotic microangiopathy; (14) pulmonary embolism (PE)–associated thrombocytopenia; (15) HIV-associated thrombocytopenia; and (16) insufficient information to classify. All charts were reviewed for limb ischemia, either arterial (absent pulses and/or radiologic/pathological evidence of artery thrombosis) or venous/microcirculatory (palpable/Doppler-identifiable pulses). In addition, we reviewed whether warfarin treatment was associated with limb ischemia and all INR values.
Coagulation factors
For 6 patients with venous limb ischemia/gangrene, we tested 52 available plasma samples (range, 4 to 11 samples per patient) for activity levels for the vitamin K–dependent procoagulant factors (II, VII, and X), as explanatory factors known to influence the INR, as well as PC activity (Protein C clotting; Siemens Healthcare Diagnostics, Marburg, Germany) and free protein S (FPS; Asserachrom FPS; Stago, Asnières-sur-Seine, France), and also a factor (factor V) not dependent on vitamin K that contributes to the INR. We also measured TAT complexes (marker of in vivo thrombin generation4 ) by enzyme-linked immunosorbent assay (ELISA; Enzygnost TAT; Siemens), as well as other indicators of DIC (eg, fibrinogen and fibrin d-dimer). For 20/52 samples, the corresponding INR values were 3.5 or greater (“supratherapeutic” in relation to usual therapeutic INR, 2.0 to 3.0). Plasmas were sodium citrate anticoagulated (0.32%, final), double spun (1500g), and stored within 4 hours in aliquots at −70°C before testing.
By analogy with HIT complicated by warfarin-induced VLG, our hypothesis was that warfarin-induced venous limb ischemia complicating cancer would be associated with marked thrombin generation (elevated TAT complexes) together with severe deficiency of natural anticoagulant, PC. To evaluate the specificity of this laboratory profile, 20 blood samples from 20 noncancer patients with supratherapeutic INRs (≥3.5) on warfarin therapy obtained from a study11 evaluating coagulation factors measured pre-/postinfusion of prothrombin complex concentrates (PCCs) were studied.
HIT antibody testing
Antiphospholipid antibodies
For 7 of our 10 patients with cancer-associated VLG, available serum permitted testing for antiphospholipid antibodies using 4 different immunoassays: IgM and IgG anticardiolipin, IgM and IgG anti-β2 glycoprotein-1 antibodies (QUANTA Lite; INOVA Diagnostics, San Diego, CA). (Screening for antiphospholipid antibodies was performed using immunoassays because the patients’ coagulopathies and anticoagulant treatment would interfere with testing for lupus anticoagulant.)
Clinical and laboratory features
Based on insights obtained from the index case (patient 1),7 we analyzed the following clinical and laboratory features: (1) thrombocytopenia (absolute and relative) in relation to heparin therapy; (2) rising platelet counts during heparin therapy; (3) elevated (supratherapeutic) INR values; (4) presence of symptomatic acute DVT in the limb affected by severe venous limb ischemia/gangrene; (5) progression to acral ischemic necrosis despite palpable/Doppler-identifiable pedal pulses; and (6) laboratory evidence for DIC, including baseline (preheparin) INR and partial thromboplastin time values, fibrinogen, and fibrin d-dimer levels.
Platelet count changes during low-molecular-weight heparin (LMWH)
We used the Matisse DVT clinical trial database15 to obtain information on expected platelet count changes in heparin-treated medical patients; we analyzed those patients without active cancer or cancer-related death for whom baseline, day 3, and day 6 platelet counts were available during treatment with therapeutic-dose enoxaparin.
Statistical analysis
Lind and colleagues16 have shown that the vitamin K–dependent factor concentrations are explanatory factors related linearly to the reciprocal of the INR (1/INR). Accordingly, we used univariate and multivariate linear regression models17 to fit the coagulation factor data from each of 6 individuals. We also simultaneously analyzed the data from all patients in a series of mixed-effect regression models with a random intercept to accommodate the serial dependence in the several responses within individuals.18 For each factor, we determined the proportion of explained variation.19 We report the explained variation as R2 for the individual regression models and Ω2 for the mixed-effect models.19
Approval for this study was provided by the Hamilton Integrated Research Ethics Board in accordance with the Declaration of Helsinki.
Results
Explanations for thrombocytopenia
Table 1 lists the most likely explanations for thrombocytopenia among the 100 cancer patients investigated for HIT antibodies (in 4 patients, testing for HIT was performed primarily because of thrombosis rather than thrombocytopenia). The 3 most common diagnoses were septicemia/multiorgan system failure (n = 33), postoperative thrombocytopenia (n = 24), and cancer-associated DIC (n = 17). Severe venous limb ischemia complicating DVT occurred in 10 patients, with 3 patients exhibiting PCD and 7 patients ultimately developing VLG (some of these latter patients had preceding phlegmasia); all 10 patients were classified by investigators’ consensus as having cancer-associated DIC.
Explanation for thrombocytopenia in 100 cancer patients who tested SRA-negative
| Diagnosis . | N . | Venous limb ischemia . | Limb artery thrombosis . | Any thrombosis* . | Died during hospitalization . |
|---|---|---|---|---|---|
| Cancer-associated DIC | 17 | 10 (59%) | 3 (18%) | 15 (88%) | 10 (59%) |
| Septicemia/multiorgan system failure | 33 | 1† (3%) | 0 (0%) | 4 (12%) | 25 (76%) |
| Postoperative hemodilution/consumption | 24 | 0 (0%) | 0 (0%) | 7 (29%) | 3 (13%) |
| Thrombosis without thrombocytopenia‡ | 4 | 0 | 1 | 4 | 0 |
| Nonimmune heparin-associated thrombocytopenia | 4 | 0 | 0 | 4 | 0 |
| Chemotherapy or radiation related | 4 | 0 | 1 | 2 | 0 |
| Leukoerythroblastosis/marrow replacement | 3 | 0 | 0 | 1 | 2 |
| Postthrombolytic therapy | 2 | 0 | 0 | 2 | 0 |
| Cardiogenic shock | 2 | 0 | 0 | 2 | 2 |
| Drug-induced immune thrombocytopenia (non-HIT) | 2 | 0 | 1 | 1 | 2 |
| Miscellaneous§ | 5 | 0 | 0 | 2 | 4 |
| Total | 100 | 11 (11%) | 6 (6%) | 44 (44%) | 48 (48%) |
| Diagnosis . | N . | Venous limb ischemia . | Limb artery thrombosis . | Any thrombosis* . | Died during hospitalization . |
|---|---|---|---|---|---|
| Cancer-associated DIC | 17 | 10 (59%) | 3 (18%) | 15 (88%) | 10 (59%) |
| Septicemia/multiorgan system failure | 33 | 1† (3%) | 0 (0%) | 4 (12%) | 25 (76%) |
| Postoperative hemodilution/consumption | 24 | 0 (0%) | 0 (0%) | 7 (29%) | 3 (13%) |
| Thrombosis without thrombocytopenia‡ | 4 | 0 | 1 | 4 | 0 |
| Nonimmune heparin-associated thrombocytopenia | 4 | 0 | 0 | 4 | 0 |
| Chemotherapy or radiation related | 4 | 0 | 1 | 2 | 0 |
| Leukoerythroblastosis/marrow replacement | 3 | 0 | 0 | 1 | 2 |
| Postthrombolytic therapy | 2 | 0 | 0 | 2 | 0 |
| Cardiogenic shock | 2 | 0 | 0 | 2 | 2 |
| Drug-induced immune thrombocytopenia (non-HIT) | 2 | 0 | 1 | 1 | 2 |
| Miscellaneous§ | 5 | 0 | 0 | 2 | 4 |
| Total | 100 | 11 (11%) | 6 (6%) | 44 (44%) | 48 (48%) |
Thrombotic events included DVT(s) (n = 26), limb artery thrombosis/thromboses (n = 6), myocardial infarction (n = 11), thrombotic cerebrovascular accident (n = 5), and superior mesenteric artery thrombosis (n = 1); several patients had >1 thrombotic event.
Symmetrical peripheral gangrene (ie, bilateral lower limb gangrene despite palpable arterial pulses) was observed in a patient with septicemia-associated DIC and hepatobiliary failure (obstructive jaundice secondary to nonresectable pancreatic cancer).
Four patients were investigated for HIT antibodies because of thrombosis without thrombocytopenia.
Miscellaneous categories include HIV-associated thrombocytopenia (n = 1), lymphoma-associated hematophagocytosis (n = 1), intracardiac tumor (n = 1), and 2 patients with insufficient information available for classification.
Clinical features of cancer-associated venous limb ischemia
Table 2 summarizes the key clinical and laboratory features of the 10 patients (mean age, 62 years) with severe venous limb ischemia. All 10 patients were ultimately diagnosed as having metastatic cancer and were additionally diagnosed (either in real time or in retrospect) as having had cancer-associated DIC. All 10 patients were receiving warfarin at the onset of severe venous limb ischemia, with a supratherapeutic INR (median = 6.5 [range, 4.2 to 9.6]). The mean duration of heparin-warfarin overlap during the initial period of heparin anticoagulation was 5 days (range, 4 to 6 days). All 9 patients with available platelet count data exhibited substantial platelet count declines (median, 69% [range, 40% to 83%]) after stopping (or reducing the dose of) heparin. All 10 patients exhibited increases in platelet count during 1 or more treatment courses with UFH or LMWH, including all 6 patients restarted on UFH or LMWH after HIT test results returned negative. The platelet count increases during heparin treatment were substantial and out of keeping for medical patients receiving heparin; for example, 9/10 patients (90%) exhibited at least a doubling of platelet count during a ∼1-week course of heparin anticoagulation, whereas only 14/507 (2.8%) patients in the Matisse-DVT trial who received LMWH exhibited a similar platelet count increase during a comparable time period (P < .0001).
Clinical picture of 10 patients with cancer-associated severe venous limb ischemia
| Pt no. . | Age/ sex . | Cancer . | Initial thrombosis/ thromboses . | Platelet count (×109/L) increase on heparin; heparin course 1, 2, or 3 . | Platelet count fall (%) off heparin (nadir) . | Thrombotic event(s) during warfarin; warfarin course 1 or 2 . | Peak INR . |
|---|---|---|---|---|---|---|---|
| 1 | 66F | Lung | CVA, DVT-R | 1, yes (328 to 682) | 1, 82% (121) | 1, PE, DVT-L→ VLG-L | 7.2 |
| 2 | 46M | Unknown | DVT-R | 1, yes (232 to 493) | 1, 66% (166) | 1, PCD-R | 6.5 |
| Primary*† | 2, yes (166 to 714) | 2, 83%‡ (80) | 2, VLG-R | 4.0 | |||
| 3, yes (80 to 667) | |||||||
| 3 | 78M | Pancreatic*† | DVT-R | 1, yes (102 to 205) | 1, 70% (61) | 1, VLG-R | 6.6 |
| 4 | 68F | Gastric*† | DVT-R, PE | 1, NA | 1, 40% (101) | 1, VLG-R | 9.6 |
| 2, yes (101 to 202) | 2, 36% (130) | ||||||
| 5 | 69F | Ovarian*† | DVT-R | 1, yes (211 to 313) | 1, 48% (164) | 1, PCD-R, WISN | 4.6 |
| 6 | 49F | Ovarian*† | CVA, DVT-L | 1, yes (138 to 703) | 1, 63% (257) | 1, VLG-L, AKA | 4.5 |
| 2, yes (257 to 1096) | 2, 64%‡ (319) | ||||||
| 7 | 64M | Lung* | DVT-R | 1, yes (353 to 571) | 1, 86% (50) | 1, PCD-R | 6.5 |
| 2, yes (50 to 545) | 2, VLG-R, BKA | 3.9 | |||||
| 8 | 61F | Lung† | DVT-R, DVT-L | 1, NA (outpatient) | 1, 69% (48) | 1, PCD-R§ | 4.6 |
| 2, yes (48 to 206) | |||||||
| 9 | 51M | Lung*† | DVT-L | 1, NA (outpatient) | 1, NA (145) | 1, PCD-L | 4.2 |
| 2, yes (145 to 564)|| | |||||||
| 10 | 64M | Pancreatic* | CVA, DVT-L, PE | 1, yes (97 to 304) | 1, 60% (110) | 1, MI, VLG-L | 8.9 |
| Pt no. . | Age/ sex . | Cancer . | Initial thrombosis/ thromboses . | Platelet count (×109/L) increase on heparin; heparin course 1, 2, or 3 . | Platelet count fall (%) off heparin (nadir) . | Thrombotic event(s) during warfarin; warfarin course 1 or 2 . | Peak INR . |
|---|---|---|---|---|---|---|---|
| 1 | 66F | Lung | CVA, DVT-R | 1, yes (328 to 682) | 1, 82% (121) | 1, PE, DVT-L→ VLG-L | 7.2 |
| 2 | 46M | Unknown | DVT-R | 1, yes (232 to 493) | 1, 66% (166) | 1, PCD-R | 6.5 |
| Primary*† | 2, yes (166 to 714) | 2, 83%‡ (80) | 2, VLG-R | 4.0 | |||
| 3, yes (80 to 667) | |||||||
| 3 | 78M | Pancreatic*† | DVT-R | 1, yes (102 to 205) | 1, 70% (61) | 1, VLG-R | 6.6 |
| 4 | 68F | Gastric*† | DVT-R, PE | 1, NA | 1, 40% (101) | 1, VLG-R | 9.6 |
| 2, yes (101 to 202) | 2, 36% (130) | ||||||
| 5 | 69F | Ovarian*† | DVT-R | 1, yes (211 to 313) | 1, 48% (164) | 1, PCD-R, WISN | 4.6 |
| 6 | 49F | Ovarian*† | CVA, DVT-L | 1, yes (138 to 703) | 1, 63% (257) | 1, VLG-L, AKA | 4.5 |
| 2, yes (257 to 1096) | 2, 64%‡ (319) | ||||||
| 7 | 64M | Lung* | DVT-R | 1, yes (353 to 571) | 1, 86% (50) | 1, PCD-R | 6.5 |
| 2, yes (50 to 545) | 2, VLG-R, BKA | 3.9 | |||||
| 8 | 61F | Lung† | DVT-R, DVT-L | 1, NA (outpatient) | 1, 69% (48) | 1, PCD-R§ | 4.6 |
| 2, yes (48 to 206) | |||||||
| 9 | 51M | Lung*† | DVT-L | 1, NA (outpatient) | 1, NA (145) | 1, PCD-L | 4.2 |
| 2, yes (145 to 564)|| | |||||||
| 10 | 64M | Pancreatic* | CVA, DVT-L, PE | 1, yes (97 to 304) | 1, 60% (110) | 1, MI, VLG-L | 8.9 |
All 10 patients were diagnosed as having metastatic cancer. All 10 patients tested negative for HIT in the SRA; additionally, patients 1, 6, 7, 8, 9, and 10 tested negative in the IgG-specific PF4/heparin ELISA; whereas patient 4 tested positive by ELISA (but did not have HIT based on the negative SRA and platelet count increase when UFH was restarted following the negative SRA test result). Only patient 3 tested strongly positive by PF4/heparin ELISA (3.24 units; normal <0.45 units), but the SRA was repeatedly negative, and cancer-associated DIC was judged a more probable diagnosis than HIT. No serum was available from patients 2 and 5 for testing in the PF4/heparin ELISA.
AKA, above-knee amputation; BKA, below-knee amputation; CVA, cerebrovascular accident (thrombotic stroke); F, female; L, left; M, male; MI, myocardial infarction; NA, not available; Pt, patient; R, right; UFH, unfractionated heparin; WISN, warfarin-induced skin necrosis (ie, central or nonacral skin necrosis).
Diagnosis of cancer was not known or suspected at time of presentation of initial thrombosis.
Pathology was available and showed adenocarcinoma (except patient 5, which showed ovarian clear cell carcinoma). For patients 1, 7, and 10, for whom pathology was not available, clinical and radiologic features were strongly indicative of metastatic cancer (which was diagnosed by the attending physicians), and which was not pathologically proven in part because of the aggressive thrombotic events, including limb ischemic necrosis, which resulted in decision for palliative treatment rather than further investigations and therapy.
Abrupt platelet count fall and thrombotic event (PE, patient 2; DVT-R, patient 6) while heparin was interrupted for biopsy.
Although progression of both R and L DVT occurred while on warfarin, PCD occurred in the R limb, which had more extensive thrombosis (from calf veins to common femoral vein) than L limb (from calf veins to superficial femoral vein).
Thrombotic event (DVT-R) without thrombocytopenia exacerbation within 24 hours of holding danaparoid for bronchoscopy/biopsy.
Representative cases
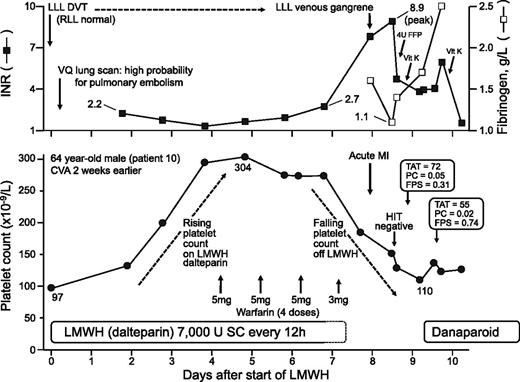
Figure 1 shows a representative case (patient 10), a 64-year-old male with a recent thrombotic stroke who presented with left lower-limb DVT treated with dalteparin/overlapping warfarin; the LMWH was stopped when the INR rose to 2.7, but 2 days later, and in association with a rapidly rising INR that peaked at 8.9, the DVT progressed to VLG. Additional clinical features included baseline thrombocytopenia (platelet count, 97 × 109/L) with a substantial rise in platelet count (to 304 × 109/L) during LMWH, and a 60% decrease in platelet count to 110 × 109/L after stopping LMWH. Additional laboratory features consistent with DIC included baseline (prewarfarin) elevation in INR (2.2) that corrected with LMWH, hypofibrinogenemia (fibrinogen nadir, 1.1 g/L, with increase to 2.5 g/L during danaparoid anticoagulation), and elevated fibrin d-dimer levels (not shown). Laboratory data indicating a profound disturbance in procoagulant-anticoagulant balance included greatly elevated TAT levels (72 and 55 ng/mL; normal, <4.2 ng/mL), despite a “therapeutic” INR on warfarin anticoagulation. Moreover, there was concomitant marked decrease in PC activity levels (0.05 and 0.02 U/mL; normal, 0.71 to 1.39 U/mL), with moderately reduced FPS of 0.31 U/mL (normal, 0.62 to 1.42 U/mL). Testing for HIT antibodies was negative. Metastatic pancreatic cancer (adenocarcinoma) was subsequently diagnosed.
Representative case (patient 10). See “Representative cases” for further details. FFP, fresh frozen plasma; LLL, left lower limb; RLL, right lower limb; SC, subcutaneous; vit K, vitamin K; VQ, ventilation-perfusion.
Representative case (patient 10). See “Representative cases” for further details. FFP, fresh frozen plasma; LLL, left lower limb; RLL, right lower limb; SC, subcutaneous; vit K, vitamin K; VQ, ventilation-perfusion.
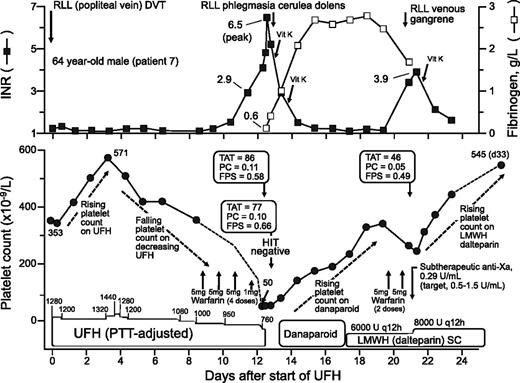
Figure 2 shows another representative case (patient 7), a 64-year-old male who presented with RLL DVT treated with therapeutic-dose UFH with overlapping warfarin; the (partial thromboplastin time adjusted) UFH dosing was reduced during overlap; when the INR rose to 2.9, the warfarin dose was reduced to 1 mg, but within 24 hours, the INR rose to 6.5, the platelet count fell to 50, and the limb affected by DVT exhibited PCD. HIT was suspected, vitamin K given (twice) to correct the INR, and danaparoid anticoagulation was commenced, but when HIT test (performed using day 12 serum) returned negative (day 17), dalteparin was commenced; the platelet count, which began to increase during danaparoid anticoagulation, continued to rise during LMWH treatment. Warfarin was resumed and the INR rose to 3.9 with progression to RLL venous gangrene. Additional clinical features included a substantial rise in platelet count (from 353 to 571 × 109/L) during preceding UFH therapy, as well as a recurrent rise in platelet count (from 50 to 545 × 109/L) during subsequent treatment with danaparoid/LMWH. Additional laboratory features consistent with DIC included hypofibrinogenemia (fibrinogen = 0.6 g/L) that recovered during subsequent anticoagulation with danaparoid, and elevated fibrin d-dimer levels (not shown). Data indicating profoundly disturbed procoagulant-anticoagulant balance included greatly elevated TAT levels (86, 77, and 46 ng/mL; normal, <4.2 ng/mL) at a time when PC activity levels were markedly decreased (0.11, 0.10, and 0.05 U/mL, respectively); concomitant FPS levels were mildly reduced or normal (0.58, 0.66, and 0.49 U/mL, respectively). Metastatic lung cancer was subsequently diagnosed.
Representative case (patient 7). See “Representative cases” for further details. anti-Xa, anti–factor Xa; PTT, partial thromboplastin time.
Representative case (patient 7). See “Representative cases” for further details. anti-Xa, anti–factor Xa; PTT, partial thromboplastin time.
Schematic picture of cancer-associated venous limb ischemia
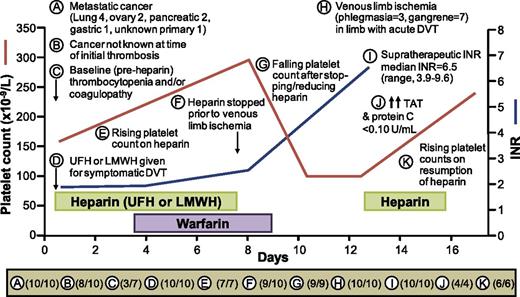
Figure 3 summarizes the characteristic clinical profile of the 10 patients identified with cancer-associated severe venous limb ischemia/gangrene. For 8/10 (80%) patients, the diagnosis of cancer was not known or suspected at initial DVT presentation. Adenocarcinoma was identified in 6/7 cases for which pathology was available (the single exception was clear cell carcinoma of the ovary). In all evaluable patients, the platelet count rose during UFH or LMWH treatment, with a fall after stopping heparin. Progression of DVT to severe venous limb ischemia occurred during warfarin treatment associated with an increase in the INR to a supratherapeutic level. With resumption of heparin, the platelet count subsequently rose. Interestingly, 2 patients developed an abrupt platelet count fall, and a thrombotic event, when heparin was briefly held to permit biopsy to diagnose cancer (patients 2 and 6; see Table 2). The clinical profile summarized in Figure 3 is distinct and, to our knowledge, represents a novel clinical syndrome.
Schematic picture of 10 cancer patients with warfarin-associated venous limb ischemia. For 11 different clinical or laboratory features, labeled “A” through “K”, the number of patients illustrating that feature (numerator) among evaluable patients (denominator) is shown at the bottom of the figure. Note that for 8 of 10 patients (B), a diagnosis of cancer was not known or suspected at the time the patient presented with DVT. The reasons why the denominator is <10 for some features is as follows: (E and G) platelet count measurements not available (eg, outpatient treatment); (I and J) plasma samples not available (note that whereas plasma samples from 6 available patients showed elevated TAT levels, samples from only 4 patients were available from the time of onset of venous limb ischemia/gangrene; however, 4/4 patients showed PC activity levels ≤0.10 U/mL).
Schematic picture of 10 cancer patients with warfarin-associated venous limb ischemia. For 11 different clinical or laboratory features, labeled “A” through “K”, the number of patients illustrating that feature (numerator) among evaluable patients (denominator) is shown at the bottom of the figure. Note that for 8 of 10 patients (B), a diagnosis of cancer was not known or suspected at the time the patient presented with DVT. The reasons why the denominator is <10 for some features is as follows: (E and G) platelet count measurements not available (eg, outpatient treatment); (I and J) plasma samples not available (note that whereas plasma samples from 6 available patients showed elevated TAT levels, samples from only 4 patients were available from the time of onset of venous limb ischemia/gangrene; however, 4/4 patients showed PC activity levels ≤0.10 U/mL).
For all 10 patients, venous limb ischemia/gangrene occurred only in 1 limb in which there had been a recent diagnosis of DVT. Interestingly, for 3 of the 10 patients, lower-limb DVT was bilateral, but venous limb ischemia/gangrene occurred only in the limb with the most recently diagnosed DVT (n = 2) or in the limb with the greater burden of thrombosis, as shown by ultrasound (n = 1). This suggests that acuity of DVT and/or burden of thrombosis contributes to risk for venous limb ischemia/gangrene.
Disturbed procoagulant-anticoagulant balance
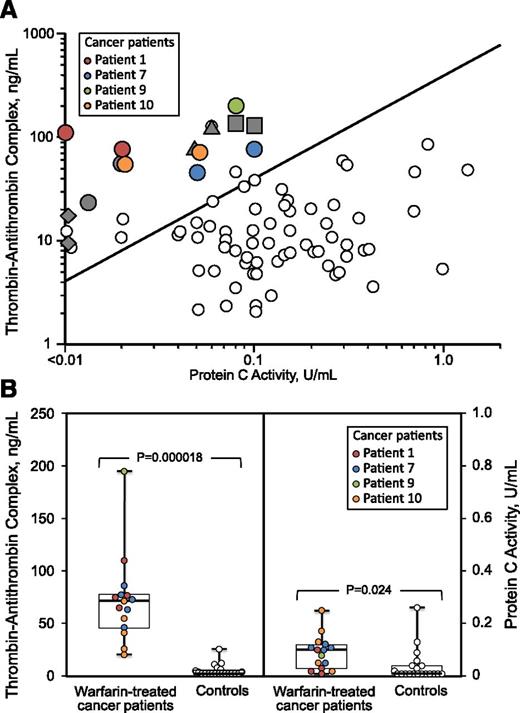
Figure 4A shows TAT and PC activity levels for 4 cancer patients for whom blood samples were available at onset of venous limb ischemia. For comparison, previously reported data4 are shown for blood samples obtained from 16 patients who received warfarin for treatment of HIT, including 4 patients who developed severe warfarin-associated venous limb ischemia/gangrene. For the 8 patients (4 with cancer, 4 with HIT) for whom multiple blood samples were available, we show the 2 values for each patient with the highest ratios of TAT/PC activity. The data show that for patients with warfarin-associated venous limb ischemia/gangrene, whether associated with cancer or with HIT, ratios of TAT/PC activity are high, consistent with profoundly disturbed procoagulant-anticoagulant balance.
Disturbed procoagulant-anticoagulant balance: TAT complexes vs PC activity. (A) Four patients with cancer-associated venous limb ischemia (7 color symbols) compared with 4 patients with HIT-associated VLG (8 solid gray symbols). For each of 8 patients with warfarin-associated venous limb ischemia (4 with cancer, 4 with HIT), the (maximum) 2 plasma samples showing the highest TAT/PC ratios are shown. For comparison, data from a previous study4 of HIT- and warfarin-associated venous limb ischemia are shown, with the 67 small open circles indicating results using plasma samples obtained from 12 warfarin-treated HIT patients (9 with DVT) who did not develop venous limb ischemia/gangrene. (B) TAT and PC activity levels for 4 cancer patients with warfarin-associated venous limb ischemia vs 20 noncancer control patients with warfarin-associated supratherapeutic INR values entered into a study of PCC replacement. For both groups of patients, all results were obtained in samples with INR ≥3.5. For the cancer patients with warfarin-associated venous limb ischemia, the 4 colors correspond to the 4 different patients. The solid horizontal line indicates median, the boxes indicates interquartile range, and the whiskers range.
Disturbed procoagulant-anticoagulant balance: TAT complexes vs PC activity. (A) Four patients with cancer-associated venous limb ischemia (7 color symbols) compared with 4 patients with HIT-associated VLG (8 solid gray symbols). For each of 8 patients with warfarin-associated venous limb ischemia (4 with cancer, 4 with HIT), the (maximum) 2 plasma samples showing the highest TAT/PC ratios are shown. For comparison, data from a previous study4 of HIT- and warfarin-associated venous limb ischemia are shown, with the 67 small open circles indicating results using plasma samples obtained from 12 warfarin-treated HIT patients (9 with DVT) who did not develop venous limb ischemia/gangrene. (B) TAT and PC activity levels for 4 cancer patients with warfarin-associated venous limb ischemia vs 20 noncancer control patients with warfarin-associated supratherapeutic INR values entered into a study of PCC replacement. For both groups of patients, all results were obtained in samples with INR ≥3.5. For the cancer patients with warfarin-associated venous limb ischemia, the 4 colors correspond to the 4 different patients. The solid horizontal line indicates median, the boxes indicates interquartile range, and the whiskers range.
Figure 4B shows results of TAT and PC ratios for the same 4 patients with cancer-associated venous limb ischemia/gangrene, as well as 20 control plasmas obtained from (noncancer) patients with supratherapeutic INR values prior to PCC treatment. These studies show that very low PC activity levels are a feature of both patient groups; indeed, PC activity levels were higher for the patients with venous limb ischemia than in the controls (P = .024). However, patients with cancer-associated DIC differed from the controls by having significantly greater TAT levels (P = .000018).
FPS levels were only mildly reduced (0.27 U/mL or higher) in some of the cancer patients with venous limb ischemia/gangrene, including 3 who had concomitant PC activity levels that were 0.10 U/mL or less. However, for 2 other patients (patients 6 and 9, respectively), nadir FPS levels were 0.10 and 0.09 U/mL (with corresponding PC nadirs of 0.07 and 0.08 U/mL, respectively), indicating a possible role for concomitant severe FPS depletion in the pathogenesis of thrombosis in some patients.
Supratherapeutic INR as a surrogate marker for severe PC depletion: regression analyses
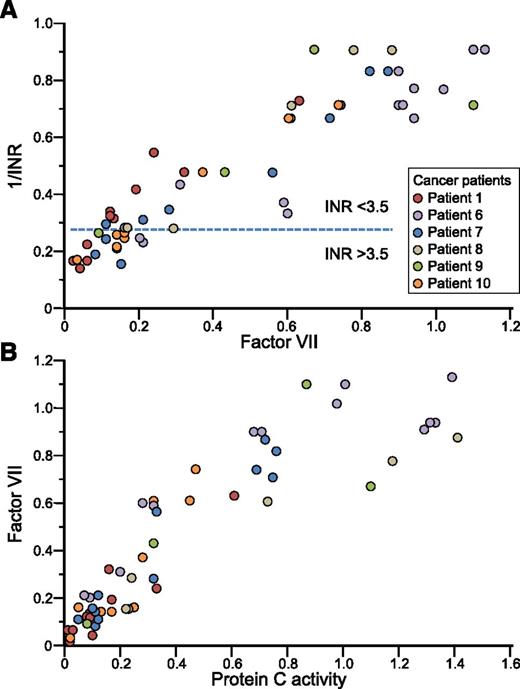
For each of the 5 patients with sufficient data to fit the models, the univariate analyses consistently demonstrated highly significant associations (P < .0001) between each explanatory factor (II, VII, X, and PC) and the response (1/INR); for the sixth patient for whom we had only 4 data points, the association between 1/INR and PC was also significant (P = .01). For PC and 1/INR, the explained variation (Ω2) for 1/INR was 78.8%, which was similar to that seen for factors X (79.6%) and II (78.0%), although not as high as that seen for VII (90.1%).
When factors VII, X, and II were considered jointly in multivariate models for each of the 5 individuals with sufficient data, factor VII retained significance for 4 of the 5 individuals and was associated with the greatest amount of explained variation in 1/INR (the R2 for VII in individual patients ranged from 88.0% to 98.5%). Although PC was highly associated with 1/INR when considered in univariate analyses (the R2 ranged from 72.6% to 98.0% for the 6 patients), when adjusted for factors VII, X, and II, the partial R2 associated with PC only ranged from 0.02% to 3.2% across individuals, suggesting that the relation between 1/INR and PC was explained by the association between factors VII, X, and II, with the most important of these being factor VII, given the high proportion of variation (∼90%) explained by this variable in the presence of the others.
The data from all 6 individuals were then analyzed simultaneously in a series of mixed-effect regression models with a random intercept. When factors VII, X, and II were modeled jointly for their effects on 1/INR the proportion of explained variation was 91.8%, with negligible increase when PC was added to the model. In the model with all 4 factors (VII, X, II, and PC), factors VII and X were highly significant (P < .0001) and factor II (P = .1713) and PC (P = .9822) were not.
These analyses can be interpreted as follows: the strong association between PC and 1/INR is explained by parallel reduction in coagulation factors VII and X, especially the former (VII accounted for ∼90% of explained variation). Figure 5A shows a scatter plot of 1/INR vs VII activity, and Figure 5B shows a scatter plot of VII vs PC activity; for this latter plot, the explained variation (Ω2) was 81.9% (P < .0001). These findings indicate that the reduction in factor VII is the major explanation for the INR elevation in such patients. The finding of uncontrolled activation of coagulation (as indicated by the markedly increased TAT levels) shows that there are sufficient levels of coagulation factors available to produce thrombin despite the low VII levels, perhaps enhanced by the inability of PC to downregulate thrombin generation.
Supratherapeutic INR as a surrogate for depletion of protein C via parallel reduction in factor VII. (A) Reciprocal of the INR (1/INR) vs factor VII levels. The area below the horizontal dashed line indicates INR values >3.5. There was a strong association between 1/INR and VII (see “Supratherapeutic INR as a surrogate marker for severe PC depletion: regression analyses”). (B) Factor VII vs PC activity levels. There was a strong association between factor VII and PC activity levels (see text for analyses, interpretation, and discussion).
Supratherapeutic INR as a surrogate for depletion of protein C via parallel reduction in factor VII. (A) Reciprocal of the INR (1/INR) vs factor VII levels. The area below the horizontal dashed line indicates INR values >3.5. There was a strong association between 1/INR and VII (see “Supratherapeutic INR as a surrogate marker for severe PC depletion: regression analyses”). (B) Factor VII vs PC activity levels. There was a strong association between factor VII and PC activity levels (see text for analyses, interpretation, and discussion).
Despite the very low PC activity levels at the time of warfarin-associated supratherapeutic INR/severe venous limb ischemia, it appeared unlikely that congenital PC deficiency was a contributing factor, based on the following considerations. First, of the 6 patients shown to have low PC activity levels, 5 had at least 1 subsequent post–vitamin K plasma sample with PC activity >0.60 U/mL (1 patient whose PC activity level rose from 0.02 to only 0.47 U/mL post–vitamin K likely had a residual effect of warfarin, suggested by persisting INR elevation). Figure 5B shows the very wide variations in PC activity levels, ranging from very low to near normal/normal, for the 6 patients who underwent testing. Second, none of the 10 cancer patients had a prior history of venous thromboembolism. Third, none of the 10 patients had a known family history of venous thromboembolism.
Antiphospholipid antibody testing
None of 7 patients with cancer-associated venous limb ischemia with available serum tested positive for antiphospholipid antibodies.
Discussion
We report 10 patients with cancer-associated venous limb ischemia/gangrene complicating treatment of DVT. In all patients, progression to venous limb ischemia occurred after the heparin was stopped (or dose reduced) and while the patients were continuing to receive warfarin and occurred in association with a supratherapeutic INR. Moreover, venous limb ischemia occurred in the same limb with recent or concurrent symptomatic DVT. When both lower limbs had DVT, the one with the most recent DVT, or (when onset of bilateral DVT was simultaneous) the one with the greatest burden of thrombosis, progressed to venous limb ischemia/gangrene. This clinical picture thus strongly resembles that of HIT-associated VLG associated with warfarin therapy: those patients also develop venous limb ischemic necrosis after stopping heparin and during warfarin therapy associated with a supratherapeutic INR, and those patients also develop acral limb ischemic necrosis in the same limb with a recent DVT.4
A key difference between the patients in our present report and patients with HIT-associated VLG is that blood samples from HIT patients contain heparin-dependent platelet-activating antibodies, whereas the patients with cancer had negative testing for HIT antibodies. Further, the patients we report typically showed a marked increase in platelet count upon resumption of UFH or LMWH therapy, presumably as a result of the anticoagulant slowing the uncontrolled activation of coagulation that is causing platelet consumption. Indeed, it is known that cancer-associated DIC can be controlled by therapeutic-dose heparin.20,21 If our patients had had HIT, we would have expected to see a platelet count fall with initiation of heparin. In addition, several of the patients had unexplained thrombocytopenia and/or coagulopathy at presentation with “idiopathic” DVT, which together with the subsequent heparin-associated rise in platelet count, provides clues regarding the possibility of underlying cancer-associated DIC.
Studies of available plasma samples support a model of disturbed procoagulant-anticoagulant balance in the cases we report, as we have proposed in our previous studies of HIT-associated VLG.2-4 Similar to our previous reports, patients with cancer-associated venous limb ischemia exhibited the combination of a marked reduction in PC activity levels (generally, <0.10 U/mL) at a time when TAT levels were greatly elevated, during the time of maximal INR coinciding with development of severe venous limb ischemia/gangrene.
The results of plasma testing provide further insights into the explanation for the characteristic supratherapeutic INR in patients with warfarin- and cancer-associated venous limb ischemia. We found a strong association between PC activity levels and 1/INR, which supports a key pathophysiological role for severe depletion of PC activity levels in predisposing to microvascular thrombosis. However, PC activity levels do not influence the INR, so we examined factors that do affect the INR (VII, X, II, and V) to explain variability in INR values and parallel correlations with PC activity levels. In these analyses, we showed strong correlations between factor VII and, to a lesser extent, factor X in predicting for an elevated INR. Indeed, in multivariate analyses, ∼90% of the variability in 1/INR was explained by factor VII levels. Thus, given the highly collinear relationship between factor VII and PC activity levels (Ω2 = 81.9%) (Figure 5B), our observations suggest that the supratherapeutic INR is a surrogate marker for severe depletion in PC activity levels, which parallel severe depletion in factor VII levels and, to a lesser extent, factor X levels. Interestingly, factor II levels were generally much higher than factor VII and X levels, even when patients had a supratherapeutic INR, perhaps helping to explain why thrombin generation continues apace.
A clinical trial showed LMWH (dalteparin) was superior to warfarin in patients with cancer-associated DVT.22 However, for 8 of our 10 patients, the diagnosis of cancer was not apparent at onset of venous limb ischemia. Indeed, the presenting clinical picture was that of “idiopathic” DVT, which was treated with a standard regimen of UFH or LMWH with overlapping warfarin therapy (mean 5-day overlap). Our patients’ limb ischemia was not likely related to insufficient duration of overlap, as recurrent thrombocytopenia, DIC exacerbation, and DVT progression occurred even in patients who underwent a full 6-day overlap. Of note, some patients only developed VLG when a second trial of warfarin therapy was attempted. Thus, we recommend that for a patient with warfarin failure who has evidence for DIC (and where underlying cancer might be present), vitamin K antagonist therapy not be readministered, given the risk for devatastating limb loss. A limitation of our study was that cancer was not proven pathologically in 3 patients (as invasive diagnostic procedures were deemed inappropriate given the patients’ terminal conditions).
In conclusion, our study points to warfarin therapy as being a key contributing factor in explaining the evolution of DVT to acral limb ischemia (phlegmasia) and VLG in some patients with cancer-associated hypercoagulability. This disorder presents a striking clinical resemblance to HIT complicated by warfarin-induced VLG, in which warfarin fails to inhibit thrombin generation while contributing to severe depletion in PC activity levels. However, in HIT the hypercoagulable state is the result of procoagulant effects of HIT antibodies, whereas in cancer-associated VLG, the procoagulant effects are related to pathobiological consequences of cancer.
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Jo-Ann I. Sheppard for technical expertise and for preparing the figures.
M.A.C. holds a Career Investigator award from the Heart and Stroke Foundation of Ontario and the Leo Pharma Chair in Thromboembolism Research at McMaster University.
Authorship
Contribution: T.E.W. and M.A.C. were responsible for case identification, data collection, analysis, and interpretation; R.S. provided control samples and performed analysis and interpretation; R.J.C. provided statistical expertise, analyses, and data interpretation; D.A.S. provided independent review of the clinical records and abstracted key data; and all authors made substantial contributions to the concept and design of the study, were involved in the writing and critical revision of the manuscript, and gave final approval for the revision to be submitted.
Conflict-of-interest disclosure: T.E.W. has received lecture honoraria from Pfizer Canada and Instrumentation Laboratory, royalties from Taylor & Francis (Informa), and consulting fees and research funding from W. L. Gore and has provided expert witness testimony relating to HIT. M.A.C. has sat on advisory boards for Janssen, Leo Pharma, Portola, and AKP America; his institution has received funding for research projects from Leo Pharma; and he has also received lecture honoraria from Leo Pharma, Bayer, Celgene, Shire, and CSL Behring and has provided expert testimony (but not in cases involving HIT). The remaining authors declare no competing financial interests.
Correspondence: Theodore E. Warkentin, Hamilton Regional Laboratory Medicine Program, Hamilton Health Sciences, Hamilton General Site, Room 1-270B, 237 Barton St E, Hamilton, ON, Canada L8L 2X2; e-mail: twarken@mcmaster.ca.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal