In this issue of Blood, Mamonkin and colleagues1 report genetically engineered T cells with specificity for the lineage marker CD5 selectively kill T-lymphoma but not normal T cells, although both express the CD5 target antigen.
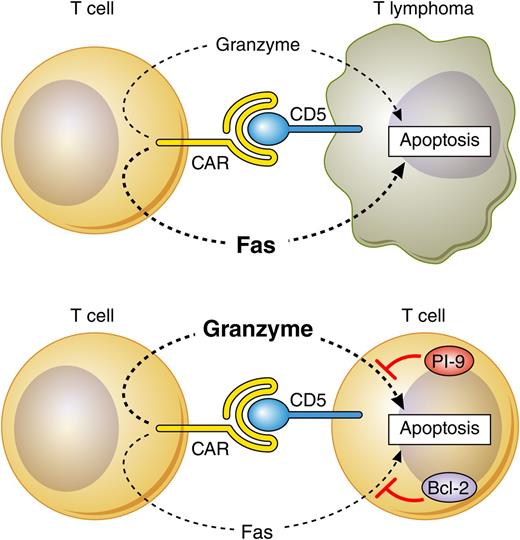
Interaction of anti-CD5 CAR T cells with CD5-expressing T-lymphoma and normal T cells triggers cytotoxic effector pathways that are effective in lymphoma but blocked by PI-9 and Bcl-2 in normal T cells. Fas/FasL is the dominant pathway mediating apoptosis in lymphoma cells, and the perforin/granzyme pathway is dominant in primary T cells. Professional illustration by Patrick Lane, ScEYEnce Studios.
Interaction of anti-CD5 CAR T cells with CD5-expressing T-lymphoma and normal T cells triggers cytotoxic effector pathways that are effective in lymphoma but blocked by PI-9 and Bcl-2 in normal T cells. Fas/FasL is the dominant pathway mediating apoptosis in lymphoma cells, and the perforin/granzyme pathway is dominant in primary T cells. Professional illustration by Patrick Lane, ScEYEnce Studios.
In the past few years, we have seen tremendous progress in the clinical application of T-cell therapy for the treatment of hematologic malignancies. Genetic-engineering technologies, based primarily on retro- and lentiviral vectors, have enabled the rapid and reliable production of therapeutic T cells with desired antigen specificity.2,3 The most dramatic success was seen with therapeutic T cells engineered to express a chimeric antigen receptor (CAR) with specificity for CD19, a lineage marker expressed in B-cell malignancies and also in normal B cells.4-6 Treatment of patients resulted in the effective elimination of malignant B cells, but required long-term antibody replacement therapy as the therapeutic T cells also killed normal B cells.
It was anticipated that a similar strategy would not work to target T-cell tumors. Redirecting T-cell specificity toward a T-cell marker may trigger mutual killing of the therapeutic T cells prior to infusion, and after infusion it may result in the elimination of endogenous T cells, leading to a severe form of immunodeficiency that, unlike B-cell deficiency, is not easily treatable.
However, in this issue of Blood, Mamonkin et al used retroviral gene transfer into primary human T cells to demonstrate that targeting the CD5 antigen enables therapeutic T cells to selectively kill human T-cell malignancies.1 This is somewhat surprising, considering that CD5 is expressed in most normal T cells and also in the immunoglobulin M–secreting B1 subset of B lymphocytes. Although gene-modified T cells expressing the anti-CD5 CAR construct were initially susceptible to mutual killing, their subsequent proliferation and continued expansion was unimpaired. Two factors contributed to the acquisition of resistance to anti-CD5 CAR-mediated killing. First, the T cells rapidly reduced the expression of the CD5 target antigen on the cell surface; second, they expressed elevated levels of molecules such as PI-9 and Bcl-2 that can protect target cells against the cytotoxic effects of the perforin/granzyme and Fas/FasL pathways that were used by the engineered effector T cells to trigger apoptosis in target cells (see figure).
When anti-CD5 CAR-engineered T cells interacted with T-lymphoma cells, this resulted in efficient killing without evidence of development of resistance. Surprisingly, anti-CD5 CAR T cells also triggered the down-modulation of CD5 on the surface of malignant cells, but compared with primary T cells, the lymphoma cells only expressed low levels of the protective PI-9 and Bcl-2 molecules. These studies revealed a novel mechanism of tumor-specific killing by antigen-specific T cells that is not dependent on the differential expression of the CAR-recognized target antigen in normal and leukemic cells, but is instead dependent on the differential expression of antiapoptotic molecules. This observation has important implications for the T-cell therapy field and suggests that the therapeutic efficacy is probably not only determined by the expression pattern of the target antigens, but also by the susceptibility of the target cells to the effector mechanisms of the therapeutic T cells.
The study by Mamonkin et al provides a basis for testing anti-CD5 CAR therapy in patients with T-cell malignancies. Possible on-target toxicity might occur in CD5-expressing thymocytes and in B1 lymphocytes. Although endogenous T cells may escape the cytotoxic effector pathways of the engineered T cells, the CD5 expression on endogenous T cells may be sufficient to stimulate cytokine production and result in cytokine-mediated toxicity similar to that seen in patients treated with anti-CD19 CAR T cells.7 In contrast to anti-CD19 CAR T cells that kill malignant and normal B cells and thus eliminate the CAR-recognized target antigen in vivo, the treatment with anti-CD5 CAR would be expected to retain normal T-cell numbers. The retention of endogenous T cells and of CD5 antigen could enhance the duration and severity of cytokine-mediated toxicity. On the other hand, it is also possible that CD5 persistence might drive chronic stimulation and the exhaustion of the anti-CD5 CAR T cells. Clinical trials will be required to define the therapeutic efficacy, the toxicity, and the fate of engineered T cells in vivo.
Conflict-of-interest disclosure: H.J.S. is a consultant for Cell Medica and Sofinnova. He also has shares at Cell Medica.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal