Key Points
Inhibition of Myb activity by a small molecule blocks proliferation of AML cells and prolongs survival of mice in an in vivo AML model.
Abstract
The transcription factor Myb plays a key role in the hematopoietic system and has been implicated in the development of leukemia and other human cancers. Inhibition of Myb is therefore emerging as a potential therapeutic strategy for these diseases. However, because of a lack of suitable inhibitors, the feasibility of therapeutic approaches based on Myb inhibition has not been explored. We have identified the triterpenoid Celastrol as a potent low-molecular-weight inhibitor of the interaction of Myb with its cooperation partner p300. We demonstrate that Celastrol suppresses the proliferative potential of acute myeloid leukemia (AML) cells while not affecting normal hematopoietic progenitor cells. Furthermore, Celastrol prolongs the survival of mice in a model of an aggressive AML. Overall, our work demonstrates the therapeutic potential of a small molecule inhibitor of the Myb/p300 interaction for the treatment of AML and provides a starting point for the further development of Myb-inhibitory compounds for the treatment of leukemia and, possibly, other tumors driven by deregulated Myb.
Introduction
Myb, the protein encoded by the MYB proto-oncogene, is now recognized as an attractive therapeutic target for the treatment of leukemia and potentially for other human tumors.1 Myb was originally discovered as the cellular progenitor of the transforming v-Myb transduced by avian myeloblastosis virus.2,3 Myb is expressed in the hematopoietic progenitor cells, where it acts as a transcription factor to control genes important for lineage determination, cell proliferation, and differentiation.4,5 The analysis of Myb null and conditional knockout mice and of mice bearing hypomorphic Myb alleles has demonstrated that Myb is essential for most hematopoietic lineages.6-11 Myb is also expressed in several nonhematopoietic tissues,12 such as the colonic crypts, where it controls the proliferation and differentiation of the intestinal stem cells.13
Recent work has shown that deregulated Myb plays critical roles in leukemias and other types of cancer. Recurrent translocations and duplications of the Myb locus occur in acute lymphoblastic leukemia of young children.14-16 In addition, genomic rearrangements of Myb have been reported in acute myelomonocytic and basophilic leukemia.17-19 Although such rearrangements are relatively rare, they indicate that aberrant Myb expression contributes to the development of leukemia. Importantly, it has now been realized that Myb also plays essential roles in leukemias caused by genetic lesions of other genes, such as leukemias driven by human acute myeloid leukemia (AML) oncogenes.20-26 High expression of Myb is a common characteristic of these leukemias and is essential for maintenance of the leukemic cells. This was initially observed in studies with Myb antisense oligonucleotides27,28 and confirmed by more recent studies.20,29-31 An important finding that has emerged is that acute leukemia cells are “addicted” to high levels of Myb expression (i.e., they are more dependent on Myb activity than normal hematopoietic progenitor cells). This finding opens up novel therapeutic strategies for the treatment of leukemia in which partial Myb inhibition will eradicate the leukemic cells without affecting normal hematopoiesis. This idea is supported by recent studies of a mouse model of AML, which showed that short hairpin RNA-mediated downregulation of Myb resulted in remission of the leukemia without inhibiting normal hematopoiesis.30
Myb has also been implicated in the development of nonhematopoietic tumors. In estrogen receptor–positive breast cancer, Myb is highly expressed in 70% of cases.32,33 High Myb expression is observed in colon cancers and correlates with poor prognosis.34,35 Translocations between the Myb and NFIB genes occur in many adenoid cystic carcinomas, leading to the expression of Myb/NFIB fusion proteins.36 Finally, it was shown that Myb is altered by translocation in a significant percentage of diffuse low-grade pediatric gliomas.37 These observations suggest that Myb is a relevant target for the treatment of leukemia and possibly of several other types of cancer. The development of inhibitors of Myb is therefore an important step to assess the feasibility of therapeutic strategies based on inhibition of Myb.
Using a cell-based reporter system, we have recently identified the sesquiterpene lactone Mexicanin-I and several related natural compounds as the first low-molecular-weight compounds that inhibit Myb-induced gene expression at low micromolar concentrations.38,39 During this work, we have discovered that the triterpenoid Celastrol inhibits Myb activity by disrupting its interaction with the KIX domain of the coactivator p300 and demonstrate that Celastrol inhibits the proliferation of AML cells in vitro and prolongs the survival of mice in an in vivo model of AML.
Methods
Cells
HD11-C3-GFP1 cells are stable transfectants of the myelomonocytic chicken cell line HD11, expressing doxycycline-inducible chicken Myb and an enhanced green fluorescent protein (eGFP) reporter gene driven by the enhancer and promoter of the chicken mim-1 gene.38 eGFP fluorescence was measured with a fluorescence microplate reader. If not indicated otherwise, Myb-induced fluorescence was quantified by subtracting the background fluorescence of the cells measured in the absence of doxycycline from the values obtained in the presence of doxycycline. Murine hematopoietic progenitor cells were isolated from the femur of C57/BL6 wild-type and enriched on the basis of the absence of lineage differentiation markers (lin−) by immunomagnetic beads using the MACS Lineage Cell Depletion Kit (Miltenyi Biotec) as described elsewhere.40 Murine leukemias were generated by transplantation of oncogene (MLL-AF9 or MYC/BCL2)-transduced lineage-negative cells into lethally irradiated syngenic recipients as decribed.41 AML blast cells were obtained from the bone marrow of patients diagnosed with AML at the Münster University Hospital. Blasts were enriched (usually >90%) by density centrifugation. CD34+ hematopoietic progenitor cells were isolated by magnetic cell sorting with anti-CD34 antibodies (MACS, Miltenyi Biotec) from leukapheresis products of healthy donors undergoing harvest for allogeneic stem cell transplantation. All patients and donors provided written consent and all studies were approved by the local ethical board.
Differentiation and apoptosis assays
A total of 106 HL60 cells were cultured for 2 days in RPMI 1640 medium containing the desired concentration of Celastrol and/or all-trans-retinoic acid (ATRA) or LBH589. The cells were analyzed by May-Grünwald staining or by flow cytometry using phycoerythrin-labeled anti-human CD11b antibody (BD Pharmingen). For apoptosis assays, 106 HL60 cells were treated with Celastrol for 24 hours. The cells were then analyzed with the Trevigen TACS Annexin V kit (Gentaur GmbH, Aachen, Germany) according to the protocol provided with the kit. Flow cytometry analyses were always done on 104 cells. Cell viability was analyzed by a 3-(4,5 dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl-2-(4-sulfophenyl)-2H-tetrazolium assay.39
Colony formation assays
Human AML blasts and CD34+ progenitor cells were seeded in growth factor supplemented methylcellulose medium (Stem Cell Technologies, Grenoble, France). Human CD34+ cells and AML blasts were seeded as 500 to 1000 viable cells (as determined by trypan blue staining) per 3 mL per dish, respectively. All experiments were performed in triplicate. Colonies with more than 50 cells were counted on day 7. Mouse AML cells and normal hematopoietic progenitors were seeded as 500 to 1000 viable cells per 3 mL per dish.
Transplantation experiments
Animal experiments were performed under an animal project license according to UK legislation. Bone marrow cells from 8- to 12-week-old C57/BL6 (CD45.2) mice were infected with retroviruses encoding Meis1 and HoxA9.41 A total of 2.5 × 105 infected cells together with 3 × 105 normal whole bone marrow cells from the congenic strain C57/BL6 × B6:SJL (CD45.1/CD45.2) were injected into the tail vein of lethally irradiated (9 Gy) B6:SJL (CD45.1) mice as primary recipients. Secondary B6:SJL recipients were generated by transplanting 2.5 × 105 whole bone marrow cells from primary recipients into sublethally irradiated (4.5 Gy) B6:SJL mice. The secondary recipients were then treated with 0.5 mg/kg Celastrol by intraperitoneal injection 3 times a week for 4 consecutive weeks beginning at day 8 posttransplantation. Control mice were injected with phosphate-buffered saline alone. Mice were monitored daily for disease development.
Additional methods are provided as supplemental data on the Blood Web site.
Results
Celastrol inhibits Myb activity
We have recently developed a reporter cell system as a screening tool for Myb inhibitors, which is based on a chicken macrophage cell line stably transfected with a GFP reporter gene driven by the promoter and enhancer of the Myb-inducible chicken mim-1 gene,42 a doxycycline-inducible expression vector for chicken Myb and an expression vector for the Tet repressor38 (Figure 1A). Doxycycline-induced Myb expression increases the fluorescence, which serves as readout for Myb activity (Figure 1B). Using this cell line, we screened a number of plant-derived sesquiterpene lactones39 as well as several triterpenoids and naphthoquinones, which were selected for the presence of so-called α,β-unsaturated carbonyl groups, which are responsible for the biological activities of many sesquiterpene lactones. During this work, we discovered that the triterpenoid Celastrol (Figure 1C) inhibits Myb activity strongly (50% effective concentration [EC50] ∼0.85 μM) and slightly more potently than Mexicanin-I (EC50 ∼1.8 μM), which was previously shown to inhibit Myb activity.38,39 Cell viability assays showed that the inhibitory effect of Celastrol was not caused by a general toxic effect. Celastrol also inhibited the activation of the endogenous mim-1 gene (Figure 1E), demonstrating that Celastrol inhibits Myb activity also in the context of an endogenous Myb target gene. The amount of Myb was not decreased in the presence of Celastrol, indicating that Celastrol inhibits the activity and not the expression of Myb. We also confirmed the inhibitory effect of Celastrol by an artificial Myb-responsive reporter gene containing several high-affinity Myb-binding sites (Figure 2A). Overall, these experiments showed that Celastrol inhibits Myb activity at a low micromolar concentration.
Celastrol suppresses the activity of Myb. (A) Schematic illustration of the fluorescence-based reporter cell line HD11-C3-GFP1. The cells carry a stably transfected mim-1 promoter/enhancer GFP reporter gene, an expression vector for the Tet-repressor (Tet-R), and a cytomegalovirus (CMV) promoter-based expression vector for chicken Myb that contains Tet-operator sites close to the transcriptional start site (CMV*). (B) HD11-C3-GFP1 cells grown for 12 hours in the presence or absence of doxycycline (dox) were analyzed by fluorescence microscopy. (C) Structure of Celastrol. (D) The cells were grown for 12 hours in the presence of doxycycline and the indicated concentrations of Celastrol. Columns on the left show the mean GFP fluorescence with standard deviations. Columns on the right show the viability of the cells as determined by a 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide; 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide assay. The values were normalized to the fluorescence and viability of cells treated only with doxycycline. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test). (E) HD11-C3-GFP1 cells were grown for 12 hours in the presence or absence of doxycycline and Celastrol, as indicated. The cells were then analyzed by northern blotting for expression of mim-1 and ribosomal protein S17 mRNAs (upper) and by western blotting for Myb and β-actin (lower).
Celastrol suppresses the activity of Myb. (A) Schematic illustration of the fluorescence-based reporter cell line HD11-C3-GFP1. The cells carry a stably transfected mim-1 promoter/enhancer GFP reporter gene, an expression vector for the Tet-repressor (Tet-R), and a cytomegalovirus (CMV) promoter-based expression vector for chicken Myb that contains Tet-operator sites close to the transcriptional start site (CMV*). (B) HD11-C3-GFP1 cells grown for 12 hours in the presence or absence of doxycycline (dox) were analyzed by fluorescence microscopy. (C) Structure of Celastrol. (D) The cells were grown for 12 hours in the presence of doxycycline and the indicated concentrations of Celastrol. Columns on the left show the mean GFP fluorescence with standard deviations. Columns on the right show the viability of the cells as determined by a 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide; 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide assay. The values were normalized to the fluorescence and viability of cells treated only with doxycycline. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test). (E) HD11-C3-GFP1 cells were grown for 12 hours in the presence or absence of doxycycline and Celastrol, as indicated. The cells were then analyzed by northern blotting for expression of mim-1 and ribosomal protein S17 mRNAs (upper) and by western blotting for Myb and β-actin (lower).
Celastrol disrupts the cooperation of Myb with the coactivator p300. (A) QT6 fibroblasts were cotransfected with the Myb-inducible luciferase reporter gene pGL4-5xMRE(GG)-Myc (containing a cluster of high-affinity Myb binding sites), the β-galactosidase expression vector pCMVβ, and an expression vector for v-Myb. The cells were incubated for 12 hours with the indicated concentrations of Celastrol and then analyzed for luciferase and β-galactosidase activities. The columns show the average luciferase activity normalized to the β-galactosidase activity. Thin lines show standard deviations. v-Myb expression was visualized by western blotting (bottom). (B) HD11-C3-GFP1 cells grown for 12 hours in the presence or absence of doxycycline and the indicated concentrations of Celastrol, Trolox, or vitamin (vit.) C were analyzed by fluorescence microscopy. The fluorescence of cells only treated with doxycycline was set to 100%. (C) The positions of cysteine residues in v-Myb are shown schematically at the top. HD11 cells transfected with expression vectors for wild-type (wt) or the CallA mutant of v-Myb were treated for 24 hours with the indicated concentrations of Celastrol and analyzed by northern blotting for expression of the endogenous mim-1 and S17 mRNAs. (D) QT6 fibroblasts were transfected and analyzed as in (A), except that expression vectors for c-Myb and p300 were used. (E) QT6 fibroblasts were transfected with the Gal4-dependent reporter gene pG5E4-38luc, pCMVβ, and expression vectors for Gal4/Myb and KIX-VP19, as indicated. The transfected cells were incubated for 12 hours with or without Celastrol followed by analysis of reporter gene activities. The columns show the average luciferase activity normalized against the β-galactosidase activity. The luciferase activity in the Gal4/Myb and KIX-VP16 transfected cells was set to 100%. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test).
Celastrol disrupts the cooperation of Myb with the coactivator p300. (A) QT6 fibroblasts were cotransfected with the Myb-inducible luciferase reporter gene pGL4-5xMRE(GG)-Myc (containing a cluster of high-affinity Myb binding sites), the β-galactosidase expression vector pCMVβ, and an expression vector for v-Myb. The cells were incubated for 12 hours with the indicated concentrations of Celastrol and then analyzed for luciferase and β-galactosidase activities. The columns show the average luciferase activity normalized to the β-galactosidase activity. Thin lines show standard deviations. v-Myb expression was visualized by western blotting (bottom). (B) HD11-C3-GFP1 cells grown for 12 hours in the presence or absence of doxycycline and the indicated concentrations of Celastrol, Trolox, or vitamin (vit.) C were analyzed by fluorescence microscopy. The fluorescence of cells only treated with doxycycline was set to 100%. (C) The positions of cysteine residues in v-Myb are shown schematically at the top. HD11 cells transfected with expression vectors for wild-type (wt) or the CallA mutant of v-Myb were treated for 24 hours with the indicated concentrations of Celastrol and analyzed by northern blotting for expression of the endogenous mim-1 and S17 mRNAs. (D) QT6 fibroblasts were transfected and analyzed as in (A), except that expression vectors for c-Myb and p300 were used. (E) QT6 fibroblasts were transfected with the Gal4-dependent reporter gene pG5E4-38luc, pCMVβ, and expression vectors for Gal4/Myb and KIX-VP19, as indicated. The transfected cells were incubated for 12 hours with or without Celastrol followed by analysis of reporter gene activities. The columns show the average luciferase activity normalized against the β-galactosidase activity. The luciferase activity in the Gal4/Myb and KIX-VP16 transfected cells was set to 100%. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test).
Celastrol has been implicated in the induction of oxidative stress, which adversely affects the activities of many proteins.43 To study the role of oxidative stress in the inhibition of Myb, we treated the reporter cells with the antioxidants Trolox or vitamin C, However, this did not diminish the effect of Celastrol (Figure 2B), indicating that the inhibition of Myb was not mediated by reactive oxygen species. Celastrol can also act as an electrophile to generate covalent adducts with nucleophilic groups, especially thiol groups of cysteine residues.43 To see if the inhibitory activity of Celastrol was caused by alkylation of cysteine residues, we replaced all of the 7 cysteines of v-Myb with alanine. Figure 2C shows that the inhibitory effect of Celastrol on wild-type and cysteine-free v-Myb was indistinguishable, indicating that Celastrol does not inhibit Myb activity by alkylating cysteine residues. We therefore considered the possibility that Celastrol inhibits Myb indirectly.
Celastrol disrupts the Myb-p300 interaction
The activity of Myb is highly dependent on interaction with the coactivator p300.10,44 To investigate if Celastrol interferes with the cooperation of Myb and p300, we asked whether increased expression of p300 rescues Myb activity. Reporter assays demonstrated that ectopic expression of p300 abolished the inhibitory effect of Celastrol (Figure 2D). Next, we investigated if Celastrol inhibits the interaction of Myb and p300, which is mediated by the transactivation domain of Myb and the KIX domain of p300.45 Figure 2E shows that the activity of Gal4-Myb on a Gal4-dependent reporter gene was suppressed by Celastrol, indicating that Celastrol inhibits the transactivation domain of Myb. The luciferase activity was strongly increased by KIX-VP16, reflecting the Myb-KIX interaction. Interestingly, the increased activity from KIX-VP16 was also strongly inhibited by Celastrol, suggesting that Celastrol disrupts the Myb-KIX interaction.
To support this conclusion, we used an in vitro binding assay, which is based on the Autodisplay of the KIX domain on the outer membrane of Escherichia coli and a soluble GFP-Myb fusion protein that harbors the Myb transactivation domain as a binding partner (Figure 3A).46 Bacterial autodisplay provides a powerful experimental platform for the analysis of protein-protein interactions and the development of inhibitors.47,48 Figure 3B shows that bacteria, which express the KIX domain on their surface, were able to bind GFP-Myb but not GFP. The interaction of Myb and the KIX domain is mediated by an LXXLL motif located in the transactivation domain of Myb.45 Mutation of this motif, such as replacement of the Leu-302 by alanine, disrupts the interaction.10 Figure 3C shows that the L302A mutant of Myb abolished the binding, demonstrating the specificity of the binding assay. Binding experiments in the presence of Celastrol showed that addition of 1 μM Celastrol inhibited the interaction of the KIX-expressing bacteria with GFP-Myb, confirming that Celastrol disrupts the Myb-KIX interaction (Figure 3D).
Celastrol inhibits the Myb-KIX interaction. (A) The principle of bacterial autodisplay is shown on the left. A recombinant autotransporter in the outer membrane (o.m.) of E coli exposes the KIX (blue) domain on the bacterial surface, where it can bind a soluble Myb-GFP fusion protein. The domain structures of p300, the KIX-AIDA-I autotransporter, Myb, and the bacterial eGFP/Myb protein are shown on the right. DBD and TA, DNA-binding and transactivation domains of Myb; KIX, Br, HAT, and E1A refer to the KIX-, bromo-, and histone acetyltransferase domains and the E1A binding region of p300, respectively; SP, signal peptide; PAS passenger, linker, and β-barrel, the functional domains of the autotransporter. Binding experiments using bacteria expressing the KIX domain on the surface. Bacteria were incubated with eGFP/Myb or with eGFP (B), with wild-type or L302A mutant eGFP/Myb fusion proteins (C), or with wild-type eGFP/Myb fusion protein in the absence or presence of 1 μM Celastrol (D). Molecular docking studies. (E) The position of the LXXLL containing α-helix of Myb in the Myb-KIX complex is shown schematically. (F) The docking of Celastrol to the same surface of the KIX domain. The colors indicate the electrostatic potential of the binding surface (blue, positive; red, negative). (G) The interactions between Celastrol and Lys-568 and Glu-645 are highlighted.
Celastrol inhibits the Myb-KIX interaction. (A) The principle of bacterial autodisplay is shown on the left. A recombinant autotransporter in the outer membrane (o.m.) of E coli exposes the KIX (blue) domain on the bacterial surface, where it can bind a soluble Myb-GFP fusion protein. The domain structures of p300, the KIX-AIDA-I autotransporter, Myb, and the bacterial eGFP/Myb protein are shown on the right. DBD and TA, DNA-binding and transactivation domains of Myb; KIX, Br, HAT, and E1A refer to the KIX-, bromo-, and histone acetyltransferase domains and the E1A binding region of p300, respectively; SP, signal peptide; PAS passenger, linker, and β-barrel, the functional domains of the autotransporter. Binding experiments using bacteria expressing the KIX domain on the surface. Bacteria were incubated with eGFP/Myb or with eGFP (B), with wild-type or L302A mutant eGFP/Myb fusion proteins (C), or with wild-type eGFP/Myb fusion protein in the absence or presence of 1 μM Celastrol (D). Molecular docking studies. (E) The position of the LXXLL containing α-helix of Myb in the Myb-KIX complex is shown schematically. (F) The docking of Celastrol to the same surface of the KIX domain. The colors indicate the electrostatic potential of the binding surface (blue, positive; red, negative). (G) The interactions between Celastrol and Lys-568 and Glu-645 are highlighted.
Structural analysis has previously revealed that the Myb LXXLL motif forms an α-helix that binds to a hydrophobic groove on the surface of the KIX domain.45 To understand how Celastrol might inhibit this interaction, we performed molecular docking studies (Figure 3E-G). These studies suggested that Celastrol binds to the hydrophobic groove, thereby presumably preventing the Myb-KIX interaction. Binding of Celastrol to the KIX domain is mediated by hydrophobic interactions as well as by polar interactions of the carboxyl group with Lys-568 and the hydroxyl group with Glu-645 (Figure 3G).
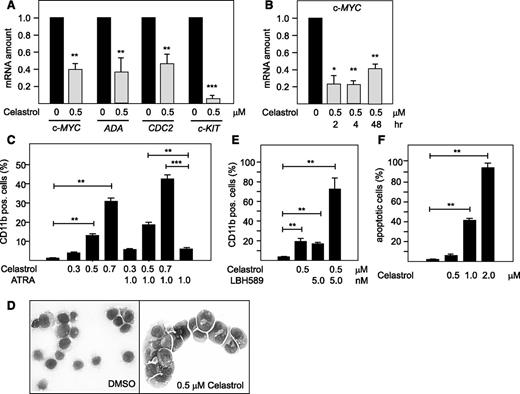
Celastrol inhibits the expression of Myb target genes and induces myeloid differentiation and apoptosis
To investigate the influence of Celastrol on hematopoietic cells expressing Myb, we used the promyelocytic leukemia cell line HL60 and examined the effect of Celastrol on the expression of several Myb target genes by real-time polymerase chain reaction (PCR), including c-MYC, ADA, CDC2, c-KIT.49-51 Figure 4A shows that the expression of all of these genes was significantly suppressed in HL60 cells treated with 0.5 μM Celastrol, confirming that Celastrol also inhibits Myb activity in human hematopoietic cells. To more convincingly demonstrate that Celastrol directly inhibits the transcription of Myb-dependent target genes and that the downregulation observed after 24 hours is not simply a consequence of the altered differentiation state of the cells, we focused on the c-myc gene, whose messenger RNA (mRNA) has an extremely short half-life.52 We analyzed c-myc mRNA levels after 2 and 4 hours when phenotypic effects are not yet observed. Figure 4B shows that Celastrol already inhibited c-myc expression after 2 hours, supporting the notion that Celastrol effectively and directly inhibits the transcription of Myb target genes.
Celastrol suppresses the expression of Myb target genes and induces myeloid differentiation and apoptosis in HL60 cells. (A) Effect of Celastrol on human Myb target genes. Real-time PCR analysis of ACTB, c-MYC, ADA, CDC2 and c-KIT expression in HL60 cells treated for 24 hours with or without 0.5 μM Celastrol. Columns show the amount of the indicated mRNAs normalized to the amount of β-actin mRNA. (B) Analysis of c-myc expression at different times of Celastrol treatment. (C) Effect of Celastrol on the differentiation of HL60 cells. Cells were treated for 2 days with the indicated concentrations of Celastrol or ATRA. Columns indicate the percentage of CD11b-positive cells, as determined by flow cytometry. (D) May-Grünwald staining of HL60 cells treated for 2 days with dimethylsulfoxide (DMSO) or 0.5 μM Celastrol. (E) HL60 cells treated for 2 days Celastrol and LBH589 were analyzed as in C. (F) HL60 cells were treated for 24 hours with the indicated concentrations of Celastrol and analyzed for staining with Annexin V. The columns indicate the percentage of apoptotic cells. Asterisks indicate statistical significance (*P < .05, **P < .01, ***P < .001, Student t test).
Celastrol suppresses the expression of Myb target genes and induces myeloid differentiation and apoptosis in HL60 cells. (A) Effect of Celastrol on human Myb target genes. Real-time PCR analysis of ACTB, c-MYC, ADA, CDC2 and c-KIT expression in HL60 cells treated for 24 hours with or without 0.5 μM Celastrol. Columns show the amount of the indicated mRNAs normalized to the amount of β-actin mRNA. (B) Analysis of c-myc expression at different times of Celastrol treatment. (C) Effect of Celastrol on the differentiation of HL60 cells. Cells were treated for 2 days with the indicated concentrations of Celastrol or ATRA. Columns indicate the percentage of CD11b-positive cells, as determined by flow cytometry. (D) May-Grünwald staining of HL60 cells treated for 2 days with dimethylsulfoxide (DMSO) or 0.5 μM Celastrol. (E) HL60 cells treated for 2 days Celastrol and LBH589 were analyzed as in C. (F) HL60 cells were treated for 24 hours with the indicated concentrations of Celastrol and analyzed for staining with Annexin V. The columns indicate the percentage of apoptotic cells. Asterisks indicate statistical significance (*P < .05, **P < .01, ***P < .001, Student t test).
Because downregulation of Myb is known to induce differentiation of immature hematopoietic cells,5 we investigated if Celastrol-treated HL60 cells undergo differentiation. The cells were cultivated with different concentrations of Celastrol, ATRA, a known inducer of differentiation of HL60 cells, or combinations of both compounds. Celastrol induced the expression of CD11b as a differentiation marker in a concentration-dependent manner in up to 30% of the cell population (Figure 4C). ATRA only weakly induced differentiation, but enhanced the activity of Celastrol. Differentiation was also confirmed by the appearance of irregularly shaped nuclei and an increase of the cell cytoplasm (Figure 4D). Ye et al53 have recently demonstrated that knockdown of Myb expression and low concentrations of histone deacetylase inhibitor LBH589 synergistically induce differentiation of U937 cells. We therefore also examined the effect of Celastrol and LBH589 on the differentiation of HL60 cells. These experiments showed that both compounds induced differentiation in synergistic manner (Figure 4E). We also examined if Celastrol induces apoptosis by measuring the fraction of Annexin V–positive cells. Figure 4F shows that Celastrol concentrations above 0.5 μM induced apoptosis in a concentration-dependent manner.
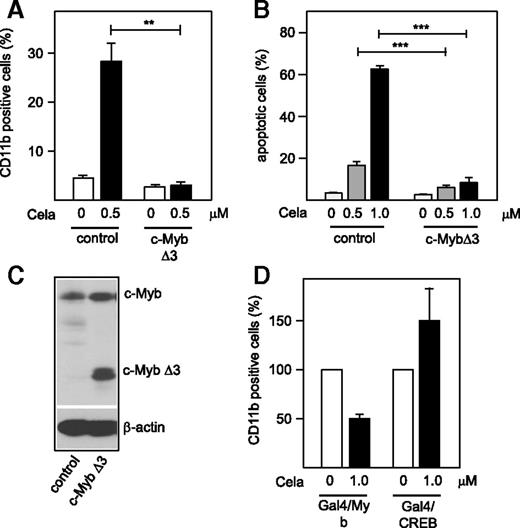
Celastrol has been implicated in various biological processes that are independent of Myb. We therefore investigated whether the effects of Celastrol on HL60 cells were due to inhibition of Myb or to a Myb-independent mechanism. To address this, we infected HL60 cells with a lentivirus expressing a C-terminally truncated Myb (c-MybΔ3). Truncation of the C terminus of c-Myb removes a negative regulatory domain, resulting a protein with enhanced transactivation and transforming potential.54 We chose to express an activated form of c-Myb as this might be more likely to counteract the inhibitory effect of Celastrol than c-Myb itself. Control cells were infected with the parental lentivirus encoding RFP. The resulting cells were then examined for the effect of Celastrol on differentiation and apoptosis; Figure 5A shows that the cells expressing ectopic Myb protein failed to differentiate in response to Celastrol, whereas the control cells differentiated. Figure 5B shows that the induction of apoptosis by higher concentrations of Celastrol was also strongly diminished in the c-MybΔ3–expressing cells. Together, these results strongly support the notion that the effects of Celastrol on differentiation and apoptosis are indeed due to inhibition of Myb.
Effect of ectopic c-Myb expression on Celastrol-induced differentiation apoptosis of HL60 cells. (A) HL60 cells infected by a control lentivirus or a lentivirus encoding c-MybΔ3 were treated for 2 days with 0.5 μM Celastrol. Columns indicate the percentage of CD11b-positive cells. (B) Lentivirally infected HL60 cells were treated for 24 hours with the indicated concentration of Celastrol and analyzed for staining with Annexin V. The columns indicate the percentage of apoptotic cells. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test). (C) Western blot analysis of total cell extracts of the cells with antibodies against Myb and β-actin. c-Myb refers to the endogenous protein. (D) QT6 cells were transfected with the Gal4-dependent reporter gene pG5E4-38luc, pCMVβ, and expression vectors for Gal4/Myb and Gal/CREB, as indicated. The transfected cells were incubated for 12 hours with or without Celastrol followed by analysis of reporter gene activities. Gal/CREB transfected cells were additionally incubated with 10 μM forskolin. The columns show the average luciferase activity normalized against the β-galactosidase activity. The luciferase activity in the absence of Celastrol was set to 100%.
Effect of ectopic c-Myb expression on Celastrol-induced differentiation apoptosis of HL60 cells. (A) HL60 cells infected by a control lentivirus or a lentivirus encoding c-MybΔ3 were treated for 2 days with 0.5 μM Celastrol. Columns indicate the percentage of CD11b-positive cells. (B) Lentivirally infected HL60 cells were treated for 24 hours with the indicated concentration of Celastrol and analyzed for staining with Annexin V. The columns indicate the percentage of apoptotic cells. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test). (C) Western blot analysis of total cell extracts of the cells with antibodies against Myb and β-actin. c-Myb refers to the endogenous protein. (D) QT6 cells were transfected with the Gal4-dependent reporter gene pG5E4-38luc, pCMVβ, and expression vectors for Gal4/Myb and Gal/CREB, as indicated. The transfected cells were incubated for 12 hours with or without Celastrol followed by analysis of reporter gene activities. Gal/CREB transfected cells were additionally incubated with 10 μM forskolin. The columns show the average luciferase activity normalized against the β-galactosidase activity. The luciferase activity in the absence of Celastrol was set to 100%.
Several other transcription factors are known to interact with the KIX domain besides Myb, challenging the specificity of the inhibitory effect of Celastrol. However, subtle differences between the binding sites or the affinities of different KIX interaction partners might affect the ability of Celastrol to disrupt these interactions.55-57 We have performed reporter gene experiments to assess the influence of Celastrol on the activity of CREB1, a transcription factor known to interact with the KIX domain in a similar but not identical manner as Myb.45 We have used a Gal4-CREB1 fusion protein containing amino acids 1 to 166 of CREB1, which encompass the binding region for the KIX domain of p300. In the presence of forskolin, Ser-133 of CREB1 is phosphorylated by protein kinase A, leading to the tight interaction of CREB1 and the KIX domain. Celastrol failed to inhibit the activity of CREB (Figure 5D), possibly because the affinity of CREB to KIX is much higher than that of Myb.45 Because Celastrol exerts pleiotropic effects that may affect signaling status of cells, we do not wish to exclude the possibility that Celastrol may affect the activity of CREB1 by indirect mechanisms. We also do not exclude the possibility that Celastrol may interfere with other interactions involving the KIX domain. Nevertheless, our data show that Celastrol does not indiscriminately inhibit all interactions of the KIX domain.
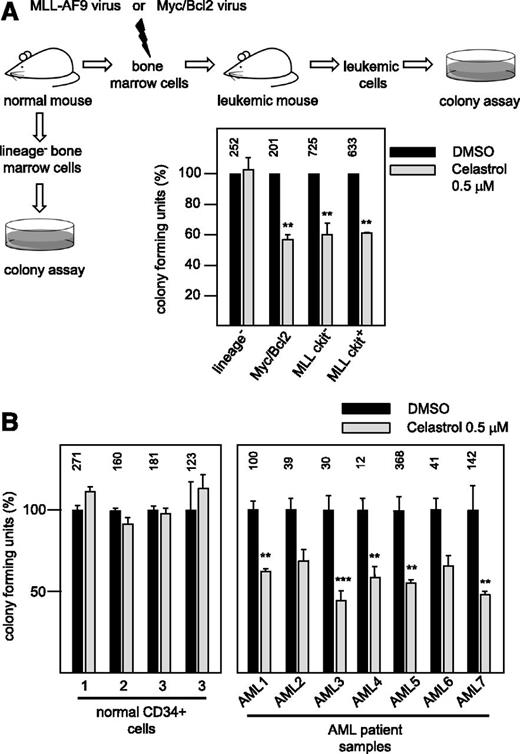
The proliferation of primary AML cells is more sensitive to Celastrol than the proliferation of normal hematopoietic progenitor cells
To investigate the effect of Celastrol on primary hematopoietic cells, we used 2 mouse models of AML that are based on retrovirally induced expression of an MLL-AF9 fusion protein58 or c-Myc/Bcl259 in hematopoietic progenitor cells. Leukemias were induced in C57BL/6 mice after transplantation of lineage-negative progenitor cells infected with MLL/AF9 or c-Myc/Bcl2 retrovirus. c-Kit–positive leukemic cells representing leukemia stem cells58 and c-Kit–negative leukemic cells were then isolated from the mice and subjected to colony formation assays in the absence or presence of 0.5 μM Celastrol. As control for normal hematopoietic cells, colony formation assays were performed with lineage-negative cells isolated from the bone marrow of healthy mice. As illustrated in Figure 6A, Celastrol suppressed colony formation of the leukemic cells, whereas colony formation of normal cells was not significantly affected.
Impact of Celastrol on the proliferation of primary AML cells and normal hematopoietic progenitors. (A) Effect of Celastrol in mouse models of AML. As outlined schematically at the top and on the left, lineage-negative cells from the bone marrow of healthy mice and primary leukemic blasts from mice were subjected to colony formation assays in the absence or presence of 0.5 μM Celastrol. Leukemias were generated by transduction of progenitor cells with Myc/Bcl2 or MLL/AF9 retroviruses. MLL/AF9-derived leukemic blasts were sorted into c-Kit–negative (bulk blast cells) and c-Kit–positive cells (leukemic stem cells) before colony formation assays were performed. Equal numbers of cells were plated with DMSO (black bars) or with Celastrol (gray bars) in each case. Columns show the relative colony number, normalized to the colony number of the DMSO control. Asterisks indicate statistical significance (**P < .01, Student t test). (B) Influence of Celastrol on primary human cells. Colony formation assay of 4 batches of CD34+ hematopoietic progenitor cells from healthy donors and leukemic blasts from 7 different AML patients. Equal numbers of cells were plated in the absence (black bars) or presence (gray bars) of 0.5 μM Celastrol. Bars show colony numbers as percent of DMSO-treated controls. The numbers above the black bars indicate the average colony number for each control sample.
Impact of Celastrol on the proliferation of primary AML cells and normal hematopoietic progenitors. (A) Effect of Celastrol in mouse models of AML. As outlined schematically at the top and on the left, lineage-negative cells from the bone marrow of healthy mice and primary leukemic blasts from mice were subjected to colony formation assays in the absence or presence of 0.5 μM Celastrol. Leukemias were generated by transduction of progenitor cells with Myc/Bcl2 or MLL/AF9 retroviruses. MLL/AF9-derived leukemic blasts were sorted into c-Kit–negative (bulk blast cells) and c-Kit–positive cells (leukemic stem cells) before colony formation assays were performed. Equal numbers of cells were plated with DMSO (black bars) or with Celastrol (gray bars) in each case. Columns show the relative colony number, normalized to the colony number of the DMSO control. Asterisks indicate statistical significance (**P < .01, Student t test). (B) Influence of Celastrol on primary human cells. Colony formation assay of 4 batches of CD34+ hematopoietic progenitor cells from healthy donors and leukemic blasts from 7 different AML patients. Equal numbers of cells were plated in the absence (black bars) or presence (gray bars) of 0.5 μM Celastrol. Bars show colony numbers as percent of DMSO-treated controls. The numbers above the black bars indicate the average colony number for each control sample.
To explore the effect of Celastrol on primary human cells, we performed colony formation assays with CD34+ cells isolated from leukapheresis samples of healthy donors and with leukemic blasts from AML patients (Figure 6B). Colony assays performed with different batches of CD34+ cells from healthy donors showed no inhibition by 0.5 μM Celastrol. In contrast, colony formation of leukemic blasts from 7 different AML patients was inhibited by Celastrol in each case. Overall, these data showed that primary murine and human AML cells are significantly more sensitive to Celastrol than normal hematopoietic progenitors.
Celastrol prolongs the survival of mice in an in vivo AML model
To assess the potential therapeutic effect of Celastrol in vivo, we used a mouse model of an aggressive AML based on retrovirally induced expression of HoxA9 and Meis1 in hematopoietic progenitor cells.41 Similar to the MLL-AF9 leukemia model, c-Myb has been shown to act as an essential downstream gene in HoxA9/Meis1-induced leukemia.20 Bone marrow cells from wild-type C57BL/6 mice were infected with HoxA9 and Meis1 retroviruses and injected into lethally irradiated BoyJ mice. Bone marrow cells from recipient mice were then used to generate secondary BoyJ transplants that were injected with Celastrol 3 times a week starting 1 week posttransplantation. No general toxicity was observed at this dose of Celastrol. Figure 7A shows that untreated mice developed AML and died within 4 weeks after transplantation, whereas Celastrol treatment increased their survival up to 10 weeks after transplantation. We used real-time PCR to determine the effect of Celastrol on Myb activity by measuring the expression of 2 Myb target genes in the bone marrow cells isolated from untreated or Celastrol-treated mice at the same time (that is, when the untreated mice became sick). We observed a significant decrease of c-myc and c-kit mRNA levels in cells derived from Celastrol-treated mice, confirming the inhibitory effect of Celastrol on Myb activity in this in vivo model (Figure 7B). Colony formation assays were also performed with bone marrow cells from untreated or Celastrol-treated mice to demonstrate the impact of Celastrol on the proliferation of the leukemic cells in the bone marrow. We observed a significant decrease in the number of colony-forming cells in the mice treated with Celastrol compared with untreated mice (Figure 7C). In addition, the proliferation potential of cells from Celastrol-treated mice was much lower than that of cells from the control mice, as shown by replating experiments (Figure 7C). Taken together, these data showed that Celastrol has a strong inhibitory effect on the proliferation of the leukemic cells in vivo and prolongs the survival of the leukemic mice.
Celastrol prolongs the survival of mice in an in vivo model of an aggressive AML. (A) Survival of mice developing a HoxA9/Meis1-induced AML. Mice were treated with Celastrol (broken line) or left untreated (solid line). (B) Effect of Celastrol on Myb target genes. Quantitative real-time PCR analysis of c-myc and c-kit mRNA expression was performed on bone marrow cells from AML-induced control mice (black bars) or Celastrol-treated mice (gray bars). Expression was normalized against ribosomal 18S RNA. (C) Replating assays of bone marrow cells from AML-induced control and Celastrol-treated mice. Total bone marrow cells from mice untreated (black bars) or Celastrol-treated (gray bars) were grown in methylcellulose without Celastrol at a concentration of 1 × 104 cells/mL. The cells were replated every 10 days at the same concentration. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test).
Celastrol prolongs the survival of mice in an in vivo model of an aggressive AML. (A) Survival of mice developing a HoxA9/Meis1-induced AML. Mice were treated with Celastrol (broken line) or left untreated (solid line). (B) Effect of Celastrol on Myb target genes. Quantitative real-time PCR analysis of c-myc and c-kit mRNA expression was performed on bone marrow cells from AML-induced control mice (black bars) or Celastrol-treated mice (gray bars). Expression was normalized against ribosomal 18S RNA. (C) Replating assays of bone marrow cells from AML-induced control and Celastrol-treated mice. Total bone marrow cells from mice untreated (black bars) or Celastrol-treated (gray bars) were grown in methylcellulose without Celastrol at a concentration of 1 × 104 cells/mL. The cells were replated every 10 days at the same concentration. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test).
Discussion
Because of recent progress in understanding the role of Myb in leukemia and other human cancers, Myb is now emerging as an attractive target for the development of small molecule inhibitors.1,38,46,60 Most acute myeloid and lymphoid leukemia cells express high levels of Myb and are more dependent on, or addicted to, Myb expression than normal hematopoietic progenitor cells.28 This has raised the possibility that inhibitors of Myb might be able to eradicate the leukemic cells while leaving normal hematopoietic progenitors unaffected. Recent studies have provided evidence that Myb coordinates a genetic program for the self-renewal of the leukemic stem cells, which is distinct from the self-renewal program of normal hematopoietic stem cells and requires high levels of Myb activity.29,30 These studies have also suggested that a relatively mild decrease of the amount of Myb is sufficient to disrupt the proliferation of leukemic cells. The development of cell-permeable chemical inhibitors of Myb is therefore an attractive strategy and important step to further explore the feasibility of Myb-based therapeutic approaches.
We have employed the cis-regulatory elements of the highly Myb-inducible mim-1 gene to establish a fluorescence-based Myb reporter cell line, which allowed us to screen compounds for Myb-inhibitory activity.38,39 By using these cells, we have previously identified plant-derived sesquiterpene lactones as the first low-molecular-weight compounds that inhibit Myb activity at low micromolar concentrations.38,39 We have now shown that Celastrol suppresses Myb activity in the reporter cell line with an EC50 value of approximately 0.85 μM. Celastrol is a natural compound isolated from the roots of Tripterygium wilfordii (Thunder God Vine), known in traditional medicine to have a variety of activities, including antioxidant and anti-inflammatory activities.61 Numerous studies have analyzed the cellular pathways affected by Celastrol and identified potential target proteins.62 Several studies have also implicated Celastrol as a potential antitumor drug for the treatment of prostate cancer and gliobastoma.63,64 So far, the biological effects exerted by Celastrol on hematopoietic cells have not been widely studied. Several reports have shown antiproliferative effects of Celastrol on the U937 leukemia cell line and on AML cells; however, the relevant molecular targets responsible for these effects have not been clearly identified.65-67
In vitro binding assays based on bacterial autodisplay and mammalian 2 hybrid experiments have shown that Celastrol blocks the interaction of Myb with the KIX domain of p300. Biochemical and genetic studies have demonstrated that the interaction of Myb and p300 plays a pivotal role for Myb activity and that mutations within the LXXLL motif or the KIX domain of p300 disrupt the interaction of both proteins, thereby affecting the development of multiple hematopoietic lineages.10,26,44,68 Structural studies have shown that the LXXLL motif forms an α-helix that binds to a hydrophobic groove on the KIX domain of p300.45 Our molecular docking studies suggest that Celastrol binds to the same hydrophobic groove of the KIX domain, thereby competing with Myb. We have recently identified another compound, Naphthol AS-E phosphate, which inhibits Myb activity in a similar manner, underscoring the “druggability” of the Myb-KIX protein-protein interaction.46
Our data show that Celastrol inhibits the expression of bona fide Myb-regulated genes and, depending on its concentration, induces differentiation or apoptosis of HL60 cells. Interestingly, the differentiation-inducing activity of Celastrol was further increased by other compounds, such as ATRA or the broad-spectrum histone deacetylase inhibitor LBH589, which synergistically induced differentiation of HL60 cells in combination with Celastrol. This suggests that it is possible to enhance the inhibitory effect of Celastrol on cell proliferation by combining it with other compounds. Importantly, we have shown that ectopic expression of a truncated and activated version of c-Myb completely abolished the effects of Celastrol on the differentiation of HL60 cells. It therefore appears that the ability of Celastrol to induce myeloid differentiation is mediated by the inhibition of Myb activity. Similarly, the induction of apoptosis by Celastrol was also diminished by ectopic expression of Myb. Thus, although Celastrol has been implicated in various Myb-independent activities, our results strongly suggest that Myb inhibition plays a major role in the effects exerted by Celastrol on myeloid cells. The mechanism by which the C-terminally truncated c-Myb counteracts the inhibitory effect of Celastrol is not entirely clear. Like full-length c-Myb, the activity of the truncated c-Myb depends on its interaction with p300, as demonstrated by the effects of point mutations in the Myb transactivation domain that are known to disrupt the Myb-p300 interaction.69 This raises the question of why Celastrol does not inhibit the activity of the truncated protein. It is possible that the increased Myb expression raises the total Myb activity in the cell above a critical level that is sufficient to counteract the inhibitory effect of Celastrol. It is also possible that the affinity of p300 to truncated c-Myb is higher than to full-length Myb and, hence, that Celastrol inhibits the truncated protein less effectively. In any case, the observation that ectopic Myb expression rescues cells from inhibition by Celastrol supports the notion that Myb is a relevant target of Celastrol in myeloid cells.
We have employed primary cells from 2 different mouse AML models to demonstrate that the ability of the leukemia cells to form colonies in semisolid medium is inhibited by submicromolar concentrations of Celastrol. Importantly, the proliferative capacity of normal hematopoietic progenitor cells from healthy mice was not inhibited under the same conditions. Similarly, colony formation assays with leukemic cells from AML patients and cells from healthy donors confirmed that proliferation of the leukemic cells was significantly inhibited by Celastrol, whereas normal progenitor cells were not affected. These findings conform to the notion that leukemic cells require higher levels of Myb activity than normal hematopoietic cells, suggesting that a “therapeutic window” might exist to allow targeting of leukemic cells by a Myb-inhibitor while maintaining normal hematopoiesis. Because so far we have analyzed the influence of Celastrol on normal hematopoietic progenitors only in vitro, further work is required to exclude effects of Celastrol on hematopoiesis in vivo.
Finally, we have employed a mouse model of an aggressive AML based on the coexpression of HoxA9 and Meis1 to initially assess the therapeutic potential of Celastrol in vivo. Similar to the MLL-AF9 leukemia model, c-Myb acts as an essential downstream gene in HoxA9/Meis1-induced leukemia.20 Our data clearly show that Celastrol-treated mice survive significantly longer after the induction of leukemia than mice not treated with Celastrol. Furthermore, the bone marrow of Celastrol-treated mice contains smaller numbers of leukemic cells, as determined by colony formation assays.
In summary, our work provides a proof of principle for the feasibility of a Myb-based therapeutic approach for the treatment of AML. Our results also underscore the importance of the Myb-KIX interaction for Myb activity and show that this interaction is amenable to inhibition by a small molecule. Because Myb is also involved in other human cancers, such as adenoid cystic carcinoma, the potential use of Myb inhibitors might not be restricted to leukemia. Last, the promising antileukemic activity of Celastrol revealed by our studies makes Celastrol a possible guide molecule for the development of more specific and potent inhibitors of the Myb-KIX interaction.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank B. Berkenfeld, B. Lindtner, and I. Rauch for technical assistance and O. Gabrielsen for plasmids.
This work was supported by grants from the Deutsche Jose Carreras Leukämie-Stiftung e.V. (K.-H.K., C-M.-T., T.J.S.), the Deutsche Krebshilfe (K.-H.K.), the Deutsche Forschungsgemeinschaft (K.-H.K., C.M.-T., W.E.B.), the Leukaemia and Lymphoma Research Foundation (J.F.), the Adenoid Cystic Carcinoma Research Foundation (K.-H.K.), and the Graduate School of Chemistry at the University of Münster (S.U.).
Authorship
Contribution: S.U., E.D., and K.-H.K. designed and performed experiments, analyzed data, and wrote the manuscript; A.C., S.S., A.J., C.S., and A.T. designed and performed experiments and analyzed data; J.J., T.J.S., C.M.-T., and J.F. designed experiments, analyzed data, and wrote the manuscript; and P.S. and W.E.B. provided patient material and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: K.-H. Klempnauer, Institute for Biochemistry, University of Münster, Wilhelm-Klemm-Strasse 2, Münster D-48149, Germany; e-mail: klempna@uni-muenster.de.
References
Author notes
S.U. and E.D. contributed equally to this work.

![Figure 1. Celastrol suppresses the activity of Myb. (A) Schematic illustration of the fluorescence-based reporter cell line HD11-C3-GFP1. The cells carry a stably transfected mim-1 promoter/enhancer GFP reporter gene, an expression vector for the Tet-repressor (Tet-R), and a cytomegalovirus (CMV) promoter-based expression vector for chicken Myb that contains Tet-operator sites close to the transcriptional start site (CMV*). (B) HD11-C3-GFP1 cells grown for 12 hours in the presence or absence of doxycycline (dox) were analyzed by fluorescence microscopy. (C) Structure of Celastrol. (D) The cells were grown for 12 hours in the presence of doxycycline and the indicated concentrations of Celastrol. Columns on the left show the mean GFP fluorescence with standard deviations. Columns on the right show the viability of the cells as determined by a 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide; 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide assay. The values were normalized to the fluorescence and viability of cells treated only with doxycycline. Asterisks indicate statistical significance (**P < .01, ***P < .001, Student t test). (E) HD11-C3-GFP1 cells were grown for 12 hours in the presence or absence of doxycycline and Celastrol, as indicated. The cells were then analyzed by northern blotting for expression of mim-1 and ribosomal protein S17 mRNAs (upper) and by western blotting for Myb and β-actin (lower).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/127/9/10.1182_blood-2015-09-668632/4/m_1173f1.jpeg?Expires=1765969305&Signature=p7oEyq5TIpO4EGgcoSlO0xea4bZ24aeip~VImZ3psEAAW3cVE59ppcIqXlGP13nT43uGm-nZ~RII4Y3rNW~f24OXdlhD94J4acYyqu6afMomotegu-0xZ-5poYMnGV3q4QfcCc4BLGlh6ijexmmhrdcf-iYhdYW0tBBUNTp7CBEb1aJD2MkujWPtLnLtldCdmTOPn6P7NgUXUhejQ2vTMuAEJUMfdHwTQSXgTNClP5q4I1eS1xvXKjN3FdYLdF88TBwkbz~AjUE2ESo2BTxGGVHqBKYY~rrQuSzIJWOIKYE2NfErhDek-MAIvmoJfw97Zn~IeLyTQoqdcd9eEm6-1w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal