Abstract
Background: Recent studies confirm the importance of upfront AHCT for MM even in the era of new agents. Previous studies have shown differences in utilization without a difference in efficacy of AHCT in Black versus White patients. No such data is available for Hispanic (H) patients, the fastest growing segment of the US population. We studied utilization and outcomes of AHCT in MM patients based on ethnicity.
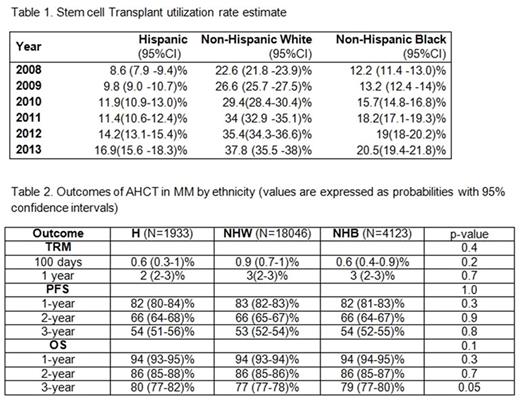
Methods: We assessed AHCT performed for MM in adults from 2008-2014 registered in the CIBMTR (N=28,450) a voluntary transplant database which captures approximately 80% of MM AHCT activity in the US. The SEER 18 database was used to estimate the incidence of MM and calculate stem cell transplant utilization rate (STUR). From this cohort, among those who received a peripheral blood with melphalan conditioning and had at least 100 days follow up data (N=24,102), we analyzed transplant-related mortality (TRM), progression-free survival (PFS) and overall survival (OS). Given the large sample size, a p value of <0.01 was considered statistically significant a priori.
Results: There were 18,046 non-Hispanic Whites (NHW), 4123 non-Hispanic Blacks (B) and 1933 H patients. The H group was younger (median age at AHCT of 57 vs. 61 years for NHW vs. 58 for B; p <0.001). Fewer patients over the age of 60 were transplanted in the H (39%) and B group (42%) vs. the NHW group (56%). More females underwent AHCT among H (43%) and B (50%) compared to NHW (41%) (p<0.001). A lower Karnofsky score (<90%) was more common in B (44%) vs. H (39%) and NHW (39). HCT-CI >3 was more common in B (38%) and NHW (34%) vs. H (24%) (p<0.001). There were more Stage III patients at diagnosis in the H (57%) vs. B (54%) and NHW (52%) (p<0.001). More H (48%) compared to 44% NHW and 45% B were in ≥VGPR pre-transplant (p=0.005).
Within the H patients, 1590 identified as H White (HW), 64 as H Black (HB) and 279 as H Other (HO). There were no differences noted for age, gender, HCT score, and pre-transplant stage between these subgroups. There was a higher number of patients with stage 3 disease noted in the HW (59%) vs. HB (55%) and HO (47%) p = 0.008.
The STUR progressively increased from 2008 to 2013 for all 3 groups but was highest for NHW (37.8%) followed by B (20.5%) and H (16.9) (Table 1). Post-transplant outcomes are shown in Table 2. On multivariate analysis, ethnicity had no effect on OS but increasing age, male gender, KPS <90, HCT-CI>3, >12 months from diagnosis to AHCT, melphalan conditioning 140 mg/m2 and <CR pre-AHCT adversely affected OS. (Figure).
Conclusions: Transplant utilization among newly diagnosed MM patients remains low overall at 25% in 2013. Although it is increasing among all ethnicities, STUR remains significantly lower among H, followed by B compared with NHW. H patients who undergo AHCT tend to be younger and fitter with worse disease. Ethnicity did not impact AHCT outcomes. Additional analyses are necessary to determine why there is a disproportion of B and H patients who fail to undergo AHCT. Further efforts are needed to increase transplant utilization for all eligible MM patients, with an emphasis on groups underutilizing transplant.
Krishnan:celgene: Consultancy, Speakers Bureau; takeda: Consultancy, Speakers Bureau; janssen: Consultancy, Speakers Bureau; onyx: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal