Abstract
Introduction: Infection is a major source of morbidity and mortality in CLL. Improved treatment efficacy and decreased immune toxicity of treatment could have altered the spectrum and consequences of infections in patients with CLL. A better understanding of infections complicating the course of non-selected patients with CLL could be useful in improving medical management.
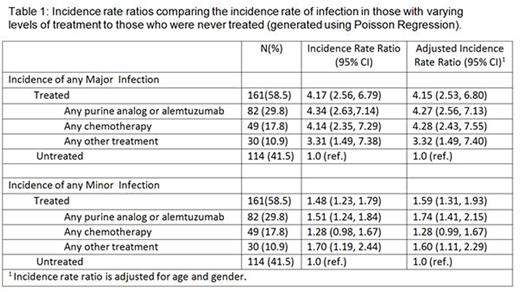
Methods: Demographic and clinical information was retrospectively extracted from medical records for clinic visits between May 1st, 2000 and May 1st, 2016 for all patients enrolled in the Wilmot Cancer Institute (WCI) CLL database. Data collected on incident infections included site, etiology, treatment, and setting of care. Major infections were defined as requiring either an inpatient stay or IV antimicrobial treatment. Minor infections were defined as any infectious episode requiring oral antimicrobials and outpatient treatment. Incidence rate ratios (IRR) were generated using Poisson regression to compare infection rates across treatment categories.
Results: Two hundred and seventy-five CLL patients contributed 937.7 person-years (p-yrs) of follow up from their first clinic visit at WCI (median follow up 2.1 yrs). Median age at diagnosis was 61.6 and only 8.2% of patients had advanced stage CLL. Most patients were CD38 negative (64.7%), ZAP70 negative (54.6%), and IGHV mutated (51.2%, n=89) and 75.1% had either 13q14 deletion as the only defect or no abnormality on FISH analysis. Sixty percent of patients needed treatment for progressive CLL; among those treated, 50.9% were ever treated with either a purine analog or alemtuzumab, 30.4% were treated with other chemotherapies, and 18.6% had non-chemotherapy treatment. B-cell receptor inhibitor (BCR) therapy was used in sixty-seven patients (63 ibrutinib, 4 idelalisib) and was the only therapy in 18 of them (BCR only).
Thirty percent of patients experienced at least one major infection (incidence rate 20.4 per 100 p-yrs) and 62.9% experienced at least one minor infection (69.3 per 100 p-yrs). The most common sites of major infections were the lower respiratory tract (7.8 per 100 p-yrs), skin (2.6 per 100 p-yrs), and urogenital tract (2.0 per 100 p-yrs). Minor infections most commonly affected the upper respiratory tract (26.8 per 100 p-yrs), skin (11.0 per 100 p-yrs, including shingles: incidence rate of 2.8 per 100 p-yrs), and bronchi (9.3 per 100 p-yrs). Patients treated for CLL had a higher risk of major infections (IRR 4.15, 95%CI 2.53, 6.80) and minor infections (IRR 1.48, 95%CI 1.23, 1.79) compared to those never treated. The age and gender adjusted risk of both major and minor infections were significantly increased by treatment with a purine analog or alemtuzumab (Table 1). The risk of major infection in the BCR only group was significantly higher than treatment-naive patients (IRR 3.31 95%CI 1.13, 9.80) and was 43% lower compared to patients treated with other modalities (IRR 0.57, 95%CI 0.21,1.55). The BCR group had a significantly higher risk of a minor infection compared to untreated patients (IRR 1.86 95% 1.14, 3.04), but had a slightly lower risk compared to those treated with other modalities (IRR 0.93 95%CI 0.57, 1.48). The BCR only group had a longer infection free survival compared to those on BCR inhibitor salvage therapy (Figure 1). An intra-patient comparison of infection risk for patients receiving BCR inhibitor salvage therapy compared to their previous chemoimmunotherapy showed an 33% increase in the risk of a major infection (IRR 1.33 95%CI 0.96, 1.86) and a 185% increased risk of a minor infection (IRR 2.85 95%CI 1.57, 5.18).
Conclusion: CLL is complicated by a large number of infections, especially in patients with progressive disease who require treatment. Minor infections contribute to considerable disease burden and can have serious sequelae (e.g. post herpetic neuralgia). Given their decreased immune toxicity profile, BCR inhibitors may decrease the risk of infections; however, this has not yet been confirmed. Our sample of CLL patients treated solely with BCR inhibitors experienced higher rates of infection compared to untreated patients. Additionally, patients treated with BCR inhibitors as salvage therapy still experienced higher rates of infection compared to their time on chemoimmunotherapy. Therefore, patients treated with BCR inhibitors should be carefully monitored for infections that can cause significant morbidity or mortality.
Barr:Pharmacyclics LLC, an AbbVie Company: Consultancy, Research Funding; AbbVie: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal