Abstract
BACKGROUND: The European Commission has granted conditional approval to daratumumab (DARA) as monotherapy in adult patients (pts) with relapsed or refractory multiple myeloma (MM) whose prior therapy included a proteasome inhibitor (PI) and an immunomodulatory agent (IMiD) and who have demonstrated disease progression on the last therapy. DARA was approved under an accelerated assessment based on single-arm phase 2 studies. Outcomes in these heavily pretreated pts in a real-world (RW) setting can provide evidence on the relative treatment efficacy of DARA versus physician's choice (PC).
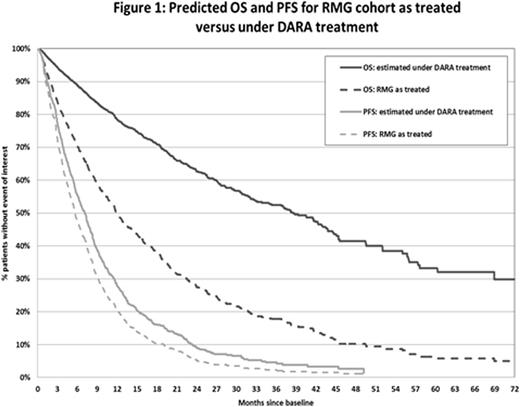
AIMS: To perform an adjusted comparison of overall survival (OS) and progression-free survival (PFS) for DARA monotherapy versus PC, as observed in a RW historical cohort of heavily pretreated and highly refractory MM pts from the Czech Republic using pt-level data.
METHODS: Using RW longitudinal pt chart data from the Registry of Monoclonal Gammopathies (RMG) of the Czech Myeloma Group, pts with ≥2 prior lines of therapy previously exposed to both a PI and an IMiD were identified. Pt-level data from the RMG were pooled from pivotal DARA monotherapy studies (pts treated with DARA 16 mg/kg). Pts in the RMG could contribute information to the analysis for multiple lines of therapy, with baseline defined as the date of initiation of the actual treatment line. For the definition of PFS, missing data for the date of disease progression for pts in the RMG who initiated subsequent therapy were replaced by the conservative proxy of the date of initiation of the next treatment. OS and PFS were analysed using a Kaplan-Meier analysis. To adjust for confounding variables, a multivariate Cox proportional hazards regression was developed that included age, gender, beta-2 microglobulin levels (β2M : <3.5/3.5-5.5/>5.5 g/L), albumin levels (<3.5/≥3.5 g/L), line of therapy (3-13), prior exposure to pomalidomide/carfilzomib, refractory status (none/double/triple/quadruple), andincidence of thrombocytopenia (defined as platelet counts <150.000 per µL) as covariates. Predicted PFS and OS curves for the RMG cohort were derived from the multivariate model.
RESULTS: From the RMG database, we identified 971 treatment lines in 463 pts previously exposed to both a PI and an IMID (n=206 in third line, n=256 in fourth line, n=203 in fifth line, n=307 in ≥sixth line). The dates of treatment initiation for the RMG pts ranged from March 2006 to March 2015. The most frequent treatment regimens were lenalidomide (33.4%), chemotherapy (18.1%), bortezomib (13.6%), thalidomide (8.0%), and bortezomib+thalidomide (5.3%). The number of pts treated with carfilzomib (2.5%) and pomalidomide (2.4%) was limited. DARA-treated pts (N=148) differed from the RMG cohort in median age (64 vs 62 years), median prior lines of therapy (5 vs 4), prior exposure to carfilzomib (41.2% vs 0.3%) and pomalidomide (55.4% vs 0.6%), thrombocytopenia incidence (46.9% vs 18.0%), and ≥triple refractory status (64.2% vs 5.3%). Median observed PFS and OS for DARA versus PC were 4.0 and 5.6 months, respectively, for PFS and 20.1 and 11.9 months, respectively, for OS. Older age, male sex, low albumin levels, high β2M levels, thrombocytopenia incidence, and double/triple/quadruple refractory status were all independent, statistically significant risk factors for mortality. Albumin levels, β2M levels, thrombocytopenia incidence, and refractory status were also predictive of PFS. The adjusted hazard ratio (95% confidence interval) for OS and PFS for DARA versus PC was 0.35 (0.22-0.56) and 0.79 (0.56-1.12), respectively. Figure 1 represents the predicted survival curves for the RMG cohort that were derived from the multivariate model, comparing observed PFS/OS versus predicted with DARA treatment.
CONCLUSIONS:
This adjusted treatment comparison suggests a significant improvement in OS and a numerical improvement in PFS for DARA compared to RW historical control data in heavily pretreated/highly refractory MM pts. The lower PFS benefit estimate for DARA compared to OS may be partly explained by limitations in the availability and comparability of data regarding progressive disease in the RMG cohort compared to clinical trial data. Adjusted comparisons between trial data and historical cohorts can provide useful insights to clinicians and reimbursement decision makers on relative treatment efficacies in the absence of head-to-head comparison studies for DARA monotherapy.
Hájek:Amgen: Honoraria, Research Funding; BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Research Funding; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Research Funding. Spicka:BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Millenium: Honoraria; Amgen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen Cilag: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Gatopoulou:Janssen Health Economics & Market Access EMEA: Employment. Vesela:Janssen Cilag s.r.o., Czech Republic: Employment. Diels:Johnson & Johnson: Employment, Equity Ownership. Besson:Janssen: Employment. Ito:Janssen: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal