Abstract
Backgrounds: Allogeneic Hematopoietic Cell Transplantation (HCT) is a potentially curative treatment for fit patients with relapsed/refractory multiple myeloma (MM). When a HLA-identical donor is not available, haploidentical HCT (haploHCT) represents an acceptable therapeutic option, especially when post-transplant cyclophosphamide (PT-Cy) is used as anti-GVHD prophylaxis.
Patients and methods: Twenty-nine patients (median age 56 years, range 47-70) undergoing myeloablative (n=15) or reduced-intensity (n=14) haploHCT from February 2011 to November 2015 are included in this retrospective analysis. The median number of previous lines of therapy was 2 (range 1-7) with 27 (93%) of patients having previously performed an autologous HCT. Both bortezomib and lenalidomide were used in 27 (92%) patients before haploHCT. Eighteen patients (62%) had chemosensitive disease at time of haploHCT (CR=4, VGPR=9, PR=5) and 11 (38%) had chemorefractory disease (PD=7, SD=4). Graft source was marrow-derived in 59% (n=17) and peripheral blood in 41% (n=12) of patients. Standard post-transplant cyclophosphamide anti-GVHD prophylaxis (50mg/mq day +3 and +4 or +5) plus mycophenolate and cyclosporine (n=24) or tacrolimus (n=3) or rapamycine (n=2) was used for the whole study cohort. Overall survival (OS) and Progression Free Survival (PFS) were performed with Kaplan-Meier analysis. Neutrophil and platelets engraftment, acute GVHD, chronic GVHD, Non-Relapse-Mortality (NRM) and Relapse Incidence/Progression of Disease (RI/POD) were obtained with competing risk analysis.
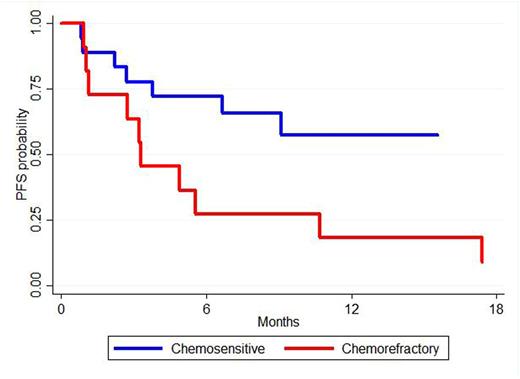
Results: At day +30, neutrophil and platelets engraftments were 86% (95%CI:65-95) and 59% (95%CI:38-74), respectively. Acute GVHD grade >2 at days +100 and +180 were 38% (95%CI: 20-55%) and 41% (95%CI: 23-59%), respectively. All grade chronic GVHD at 12 and 18 months was 21% (95%CI: 8-37. At 18 months, RI/POD was 39% (95%CI:20-58%) and NRM 15% (CI95%:5-32). With a median follow-up in survivors of 16 months (range 5-55 months), the 18-month OS and PFS were 68% (95%CI: 47-82%) and 34% (95%CI: 15-54%), respectively. Chemorefractory disease at transplant was associated with a worse 18-month RI/POD (70% vs 18%, p=<0.01) and a markedly reduced PFS (9% vs 57%, p=0.04) and OS (53% vs 78%, p=<0.01) (Figure 1). Survival outcomes were similar between marrow-derived and peripheral blood graft source cohorts.
Conclusions: HaploHCT is a feasible and effective strategy in patients with relapsed/refractory high-risk multiple myeloma. Chemorefractory disease at transplant was the only prognostic factor associated with a significant reduced RI/POD, PFS and OS.
Kaplan-Meier estimates of progression free survival from time of transplant of the chemosensitive and chemorefractory disease.
Kaplan-Meier estimates of progression free survival from time of transplant of the chemosensitive and chemorefractory disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal