Abstract
Background: Clofarabine is a second-generation purine nucleoside analogue, which has shown synergistic activity with cytarabine. We determined the maximum tolerated dose (MTD, primary endpoint), safety and efficacy (secondary endpoints) of clofarabine in combination with cytarabine and idarubicin in newly diagnosed acute myeloid leukemia (AML) patients with high-risk for induction failure stratified in two age groups (< 60 years and ≥ 60 years).
Methods: In this prospective, open-label, multicenter phase I/II study (EudraCT 2010-021719-18, CIARA trial), newly diagnosed AML patients with high risk of induction failure (NPM1 wildtype, FLT3-ITD negative), who were eligible for intensive chemotherapy, received two induction courses (cytarabine 750 mg/m2 d1-5, idarubicin 7.5 mg/m2 in patients <60 years or 6 mg/m2 in patients ≥60 years d1+3) with increasing doses of clofarabine (20-35 mg/m2 d1-5) following a 3+3 design with extension cohorts. Consolidation consisted of up to 3 courses of high-dose cytarabine or allogeneic hematopoietic cell transplantation (HCT).
Results: Forty-two patients with de novo (n=32) or secondary (n=10) AML were included. Median age was 58.5 years (range 28-73, 24 patients < 60 years, 18 patients ≥ 60 years). Intermediate/adverse risk cytogenetics were found in 22 and 12 patients, respectively (karyotype missing in 8 patients). All patients received induction 1, 27 (64%) received induction 2; 4 (10%) patients died during induction courses 1 or 2. Eight patients developed a dose-limiting toxicity (6 patients with grade 3/4 non-hematologic toxicity and 3 patients with grade 4/5 hematologic toxicity) and the MTD was determined at 30 mg/m2 clofarabine for both age cohorts (younger patients: 2 of 6 patients with DLT at 35 mg/m2, no DLT at 30 mg/m2 (n=9); older patients: 4 of 6 patients with DLT at 35 mg/m2 in the extension phase, no DLT at 30 mg/m2 (n=3). The most frequent grade 3-5 non-hematologic adverse events were febrile neutropenia, sepsis, increased liver enzymes, pneumonia, decreased appetite and diarrhea occurring in 55, 24, 21, 21, 10 and 10% of patients. The median time to neutrophils ≥0.5/nl and platelets ≥50/nl after induction 1 was 25 and 24 days, respectively. Sixteen patients (38%) proceeded to allogeneic HCT in first CR and 8 (19%) received at least one course of high-dose cytarabine consolidation.
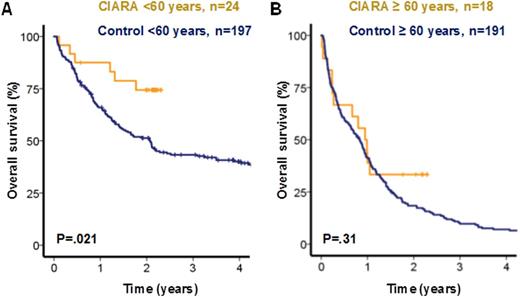
Complete remission (CR) or CR with incomplete recovery (CRi) was achieved in 67%. After a median follow up of 2.2 years the 2-year overall survival (OS) was 56% and the 2-year event-free survival was 38% (median EFS 11.4 months). Compared to a matched historical control of 197 younger AML patients (SHG 0199 trial, Schlenk et al. NEJM 2008), the CR rate was 79% in the 24 younger CIARA patients compared to 66% in the control cohort (P=.18), and 2-year OS was higher for CIARA than for control patients (74% vs 49%, P=.021, Figure A). The allogeneic HCT rate in first CR (CR1) was higher in younger CIARA compared to younger control patients (58% vs 27%, P=.002). The CR rate in older CIARA patients was 50% compared to 36% in a historical control of 191 older patients, who were selected using the same genetic inclusion criteria as for CIARA patients (HD98B trial, Schlenk et al. Haematologica 2009, P=.23). Two-year OS in older patients was similar between CIARA and control patients (33% vs 17%, P=.31, Figure B). The allogeneic HCT rate in CR1 was 11% vs 2% in CIARA vs control patients (P=.029).
Conclusion: Clofarabine can be safely administered at 30 mg/m2 in combination with cytarabine and idarubicin in younger and older newly diagnosed AML patients. Allogeneic HCT in CR1 was feasible in a high proportion of younger AML patients and likely contributed to the favorable outcome compared to historical control patients.
Overall survival in younger and older AML patients of the CIARA trial compared to historical controls.
Overall survival in younger and older AML patients of the CIARA trial compared to historical controls.
Krauter:Genzyme: Research Funding. Schlenk:Amgen: Research Funding; Pfizer: Honoraria, Research Funding. Paschka:Novartis: Consultancy; Medupdate GmbH: Honoraria; Bristol-Myers Squibb: Honoraria; Pfizer Pharma GmbH: Honoraria; Celgene: Honoraria; ASTEX Pharmaceuticals: Consultancy. Lübbert:Ratiopharm: Other: Study drug valproic acid; Celgene: Other: Travel Funding; Janssen-Cilag: Other: Travel Funding, Research Funding. Janning:Teva: Honoraria. Becker:BMS: Honoraria; Novartis: Honoraria. Heuser:Tetralogic: Research Funding; Novartis: Consultancy, Research Funding; Celgene: Honoraria; Pfizer: Research Funding; Bayer Pharma AG: Research Funding; BerGenBio: Research Funding; Karyopharm Therapeutics Inc: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal