Abstract
Donor Type and Disease Risk Predict the Success of Allogeneic Hematopoietic Cell Transplantation (HCT): A single Center Analysis of 613 Adult HCT Recipients Using a Modified Composite Endpoint
Introduction
The success of allogeneic HCT is based on long term survival, free of relapse or morbidity as commonly encountered when patients develop graft versus host disease (GVHD). The Bone marrow transplant clinical trials network (BMTCTN) recently incorporated a composite endpoint to determine success rate in ongoing clinical trials. The new composite endpoint of GVHD free, relapse free survival (GRFS) includes the factors of acute GVHD grade 3-4, relapse, death and chronic GVHD requiring systemic immunosuppression. As the decision to start patients on immunosuppression for chronic GVHD can be subjective and physician dependent, we elected to assess the success of allogeneic HCT using a more objective endpoint m-GRFS where the clinically significant negative events are acute GVHD grade 3-4, moderate-severe chronic GVHD, disease relapse and Death at 1 and 2-year post HCT.
Methods
Six hundreds and thirteen patients who underwent a first allogeneic HCT after a HLA-identical sibling (MRD, n=212), 10/10 matched unrelated donor (MUD, n=251) or T-replete haploidentical donor with post-transplant cyclophosphamide (HIDT, n=150) were included in this analysis. Patient, Disease and Transplant related variables were prospectively documented and obtained from our institutional database. The Kruksall-Wallis test was used to compare continuous variables and the Chi-squared test for categorical variables. OS, DFS and m-GRFS were estimated by the Kaplan-Meier (K-M) method. Log-log transformed confidence intervals for OS, DFS and GRFS were calculated. Comparison of m-GRFS between demographic subgroups and between clinical subgroups were evaluated using the log-rank test for the entire study period and using the Wald test for a select time point. Competing risks analysis was performed to disentangle the components of GRFS. Grade III/IV acute GVHD, mod-severe chronic GVHD, relapse and death were considered as competing risks and cumulative incidences of these endpoints were calculated. Patients were considered to have met the endpoint once any of the components occurred. Cox regression analysis was conducted to examine the impact of donor, demographic and clinical factors on the primary endpoint of modified GRFS. The proportional hazards assumption was checked by temporarily including and testing time-dependent variables and the variables in the final model passed the proportionality test. The adjusted GRFS for one characteristic was calculated as the average survival of the whole sample, assuming that everyone in the sample had this characteristic.
Results
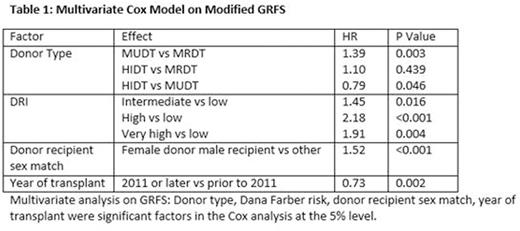
The median follow-up was 50.2 months. Patients characteristics were as follows: median age 53 years (18-77), male 56%, reduced intensity/non-ablative 49%, AML 37%, ALL 13%, MDS/MPD 24%, bone marrow graft 19%, HCT-comorbidity index >=3 in 39%, and high/very high DRI 34%. The unadjusted Kaplan-Meier estimates for 1- and 2-year m-GRFS were 36% (95%CI 32%-40%) and 28% (95%CI 25%-32%). The 2-year m-GRFS for MRD recipients was 30% (24-36%), MUD 24% (19-30%) and HIDT 33% (26-41%). The most common event at 2 years post HCT was chronic GVHD (39%) followed by relapse (31%), acute GVHD 3-4(20%) and death (10%). After adjusting for age, gender, diagnosis, conditioning intensity, donor type, cell source, HCT-CI, DRI , donor-recipient gender mismatch and year of transplant, the multivariate cox model on m-GRFS showed donor type, DRI risk , donor recipient sex mismatch and year of transplant to be significant predictors of m-GRFS (table 1). Patients who received a MUD had worse GRFS compared to MRD (HR 1.39, p=0.003) whereas HIDT had similar GRFS to MRD (HR 1.10, p=0.43). HIDT had better GRFS than MUD (HR 0.79, p=0.046). The adjusted 1- and 2- year m-GRFS showed donor type (MUD vs MRD), DRI, donor-recipient sex mismatch and transplant year to be associated with worse GRFS (table 2).
Conclusions
m-GRFS is a useful measure of transplant success. It appears to be significantly impacted by several modifiable factors including donor type, donor-recipient sex match and also by DRI. Adjusting donor choice and early referral of patients for transplant evaluation to improve DRI can potentially overcome the negative impact of these factors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal