Abstract
Introduction
There is no standard therapeutic approach for the relapse after allogeneic hematopoietic cell transplantation (allo-HCT). The aim of this paper is to confirm the role of granulocyte colony-stimulating factor (G-CSF) primed donor lymphocyte infusion (DLI) according to the timing of relapse after allo-HCT with limited CD34+ cell dose (<6x106/kg)
Methods
One hundred ten patients who had relapsed after allo-HCT at Kyungpook National University Hospital from November 2001 to December 2014, including 40 patients who received DLI from cryopreserved cells derived from the original G-CSF primed graft, were retrospectively reviewed. The patients were classified into early relapse or late relapse group by the median time of relapse after transplant.
Results
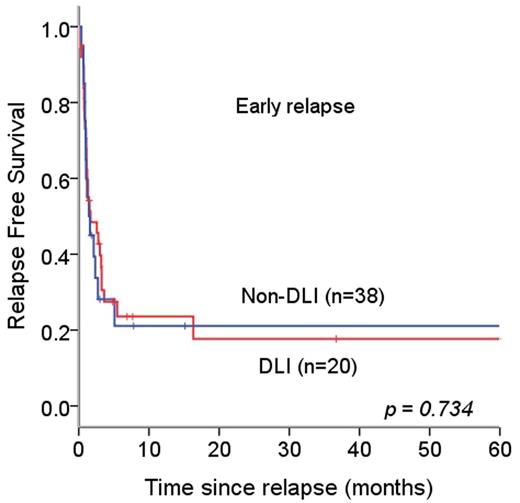
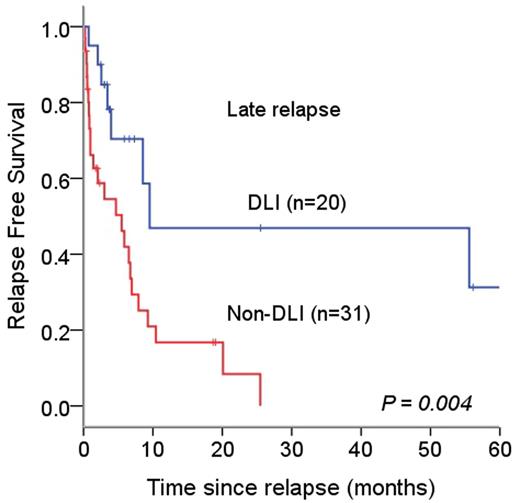
The median age at transplant was 38.5 years (range, 17-67 years) and male was 69 patients (62.2%). Primary diseases for allo-HCT included AML/MDS (n=63, 57.3%), ALL (n=32, 29.1%), CML (n=8, 7.3%), and NHL (n=7, 6.4%). Fifty four patients (49.1%) were in CR1 (complete remission), 16 (14.5%) in CR2, and 40 (36.4%) in relapsed and refractory status at the time of HCT. Sixty nine patients (62.2%) received myeloablative conditioning regimen. The median dose of CD34+ cells was 5.06x106/kg (range, 1~20.6x106/kg). Ninety nine percent of patients achieved the neutrophil recovery (> 500x103/mm3 for 3 days) at a median time of 13 days (range 9-24 days). The median time from HCT to relapse was 139 days (range, 21~1801 days). The median relapse free survival (RFS) since HCT was not significantly different according to the dose of CD34+ cells: median 147 days (range, 122-171) and 157 days (range, 87-227) in CD34+ < 6x106/kg and > 6x106/kg, respectively (p=0.249). The median overall survival (OS) since HCT was not significantly different according to the dose of CD34+ cells: median 324 days (range, 272-375) and 262 days (range, 235-288) in CD34+ < 5.06x106/kg and > 5.06x106/kg, respectively (p=0.554).The incidence of chronic GVHD was more frequent in higher CD34+ group (32.9% vs. 48.2%, P=0.042). After relapse, 57 patients (51.8%) were treated with salvage chemotherapy, 13 patients (11.8%) with second allo-HCT, and 40 patients (36.4%) with G-CSF primed DLI. The median number of CD3+T cell was 2.95x107/kg (range, 0.1~5.43x107/kg). Fourteen patients (23.6%) achieved DLI-induced CR, 20 patients progressed, and 6 patients were not evaluable for response. DLI-induced acute GVHD was observed in 25 patients (62.5%) and chronic GVHD developed in 4 patients (10%). The 1-year overall survival (OS) since relapse was not significantly different according to the use of DLI in early relapse group (11.7 +/- 5.3% and 10.0 +/- 6.7%, p=0.663), but in late relapse group, significantly higher in DLI than non-DLI (43.3 +/- 11.3% and 17.1 +/- 6.9%, p=0.021). The patients treated with DLI showed significantly higher RFS in late relapse group (286 days vs. 165 days, p=0.004). The incidence of DLI-induced GVHD did not differ between two groups.
Conclusions
G-CSF primed DLI after allo-HCT with limited CD34+ cell dose can be feasible and effective option in terms of response, donor convenience and its cost. In the late relapse group, it may replace the second transplantation for the patients with hematologic malignancies lately relapsed after first allo-HCT.
Relapse free survival according to DLI use,(A) RFS in patients experiencing early relapse of hematologic malignancies after allogeneic hematopoietic cell transplantation (B) RFS in patients experiencing late relapse of hematologic malignancies after allogeneic hematopoietic cell transplantation, DLI- donor lymphocyte infusion; RFS- Relapse free survival
Relapse free survival according to DLI use,(A) RFS in patients experiencing early relapse of hematologic malignancies after allogeneic hematopoietic cell transplantation (B) RFS in patients experiencing late relapse of hematologic malignancies after allogeneic hematopoietic cell transplantation, DLI- donor lymphocyte infusion; RFS- Relapse free survival
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal