Abstract
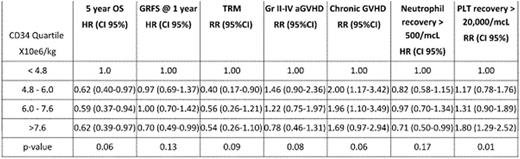
CD34+ cell dose is a critical determinant of outcomes after allogeneic PBSC transplantation, with a CD34 dose ≥2.0 x 10e6/kg shown to positively impact hematopoietic engraftment and survival. However, it is unknown whether additional benefits are observed with even higher CD34 cell doses. Therefore, we further explored the effect of intermediate, high and very high CD34 cell doses on the incidence of engraftment, acute and chronic graft-versus-host disease (GVHD) and transplant related mortality (TRM) and on probability of survival and GVHD-Relapse-free survival (GRFS). Three hundred and five consecutive patients transplanted with GCSF-mobilized PBSC from HLA-matched sibling donors (MSD) were evaluated. Patients were ≥16 years of age, had a hematological malignancy and received a myeloablative or a nonmyeloablative conditioning regimen between 2002 and 2012. The median recipient age was 52 years (r, 19-74 years) with most being male (n=194, 63.8%) diagnosed with leukemia (72%) or lymphoma (22%), and intermediate disease risk index (DRI, n=204, 67%). The median age for the donor were 49 years (r,17-76 years). In 159 patients (52%) the donor and recipient were sex matched with 89 male patients having a female door (29%). The ABO blood type was matched in 195 patients (64%), 153(50%) received a myeloablative (MA) conditioning regimen, and 37 (12%) received a reduce intensity conditioning regimen containing ATG. The median follow up of surviving patients was 793 days (r, 14-4562 days). Patients were divided in four CD34 dose quartiles: first quartile (QT1), ≤4.8 x10e6/kg, QT2 4.8-6.0 x10e6/kg, QT3 6.0-7.5 x10e6/kg, and QT4 ≥ 7.6 x 10e6/kg. Notably, the CD3 doses were similar for all quartiles: QT1 was 3.4 x 10e8/kg (r, 0.3-10.0), QT2 was 2.7 x 10e8/kg (r, 1.1-7.6), QT3 was 2.8 x 10e8/kg (r, 0.8-7.2) and QT4 was 2.8 x 10e8/kg (r, 1.4-7.7); there was no correlation between CD34 and CD3 cell doses. Patient and donor characteristics were similar in the four groups except for shorter median follow-up (P <0.01) in QT1, more sex mismatched grafts (P <0.01) in QT3, and lower median number of cell collections (P <0.01) and more female donor: male recipient pairs (P< 0.01) in QT4. Multivariate analysis results are summarized on the table. Higher CD34+ cell dose was associated with improved platelet recovery with trends toward lower TRM and improved overall survival. Chronic GVHD however was also higher. In summary, additional studies are needed to establish a survival benefit in recipients of higher cell doses >4.8 x 10e6 CD34 cells/kg. Unless survival is positively impacted, the higher risk of chronic GVHD would argue for assigning an upper CD34 cell dose limit to reduce this risk that can significantly impair quality of life.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal