Abstract
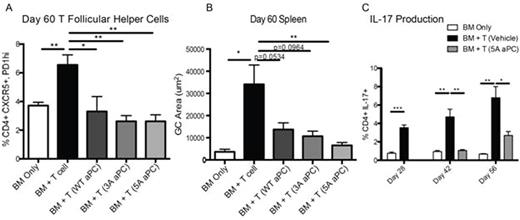
Activated Protein C (APC), a trypsin-like plasma serine protease, exerts multiple beneficial pharmacological activities, and an APC variant with reduced anticoagulant activity, namely 3A-APC (Lys191-193Ala), is in phase 2 clinical trials for ischemic stroke. Although APC's beneficial effects on endothelial, epithelial, and neuronal cells have been well described, little is known about APC's effects on the immune system. Here we study APC's immunosuppressive actions using a multi-organ system murine chronic graft versus host disease (cGVHD) model with bronchiolitis obliterans (BO) and fibrosis. To determine whether APC has in vivo immune suppressive activity, mice were conditioned with high dose cyclophosphamide and total body irradiation followed by MHC-disparate bone marrow and splenocytes. Recombinant murine APC (6 µg/dose) or vehicle was administered intraperitoneally once daily from d28-56. Three forms of APC were studied: wild type (WT)-APC and two APC variants with greatly reduced anticoagulant activity but normal cell signaling activity, 3A-APC and 5A-APC (Lys191-193Ala plus Arg229-230Ala). Pulmonary function tests (compliance, resistance and elastance) indicative of cGVHD BO were markedly improved by WT-APC and both anti-coagulant defective mutants, 3A-APC and 5A-APC. Additionally, WT-APC and the variants, 3A-APC and 5A-APC, significantly reduced pulmonary fibrosis. The lack of difference in efficacy between WT and the signaling selective variants suggests APC-induced signaling, not anticoagulant activity, is primarily responsible for reduction of pulmonary pathology in cGVHD. APC treatment also significantly reduced splenic germinal center (GC) size as well as Tfollicular helper cell (CD4+CXCR5+PD1hi) and Th17 frequencies (Figure), keys for GC formation and subsequent fibrosis. Together, these data indicated that APC-induced signaling is primarily responsible for reduction of pulmonary pathology in cGVHD.
Previous work has documented APC's antithrombotic, anti-inflammatory, anti-apoptotic, endothelial barrier stabilizing, and regenerative activities. Although receptors on multiple cell types have been implicated for APC's cell signaling activities, in the current major paradigm, endothelial cell protein C receptor (EPCR)-bound APC cleaves protease activated receptor (PAR) 1 at Arg46 to initiate arrestin-dependent biased signaling. In contrast, thrombin's canonical cleavage at Arg41 in PAR1 induces G-protein-dependent pro-inflammatory signaling. To determine if APC's benefits for cGVHD might require PAR1 cleavage at Arg41 or Arg46, we used ES cells and homologous recombination to generate C57BL/6 strains carrying the PAR1 mutation of either Arg41Gln (R41Q) or Arg46Gln (R46Q). Then donor T cells were prepared from each genetically altered strain carrying WT-PAR1, QQ41-PAR1, or QQ46-PAR1, and they were used to induce cGVHD. 5A-APC reduced cGVHD for transplanted T cells carrying WT-PAR1 and QQ41-PAR1, but it was completely ineffective for transplanted QQ46-PAR1 T cells, proving Arg46 in PAR1 in donor T cells is essential for 5A-APC's benefits. Since APC's cleavage at Arg46 is key for triggering PAR1 biased signaling, we infer that APC's benefits for cGVHD require, at least in part, direct biased activation of PAR1 on donor T cells and that this signaling precludes sufficient IL17 generation and GC formation to cause cGVHD.
In summary, daily therapy using recombinant APC was highly effective in treating ongoing cGVHD in a BO model. Studies using signaling-selective APC mutants and donor T cells obtained from novel PAR1-genetically modified mice suggest that the mechanisms responsible for cGVHD suppression involve APC-induced signaling dependent on PAR1 cleavage at Arg46 on donor T cells, and not APC's anticoagulant activity. Such signaling resulted in suppression of Tfollicular helper cells and Th17. Given the safety and efficacy record of 3A-APC in phase 1 clinical studies, these data strongly support the consideration of 3A-APC or 5A-APC for treatment of cGVHD with BO manifestations that have been refractory to other therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal