Key Points
HDAC6 inhibition represents a novel strategy to improve the efficacy of anti-CD20 mAbs.
HDAC6 inhibition increases CD20 levels by enhancing CD20 protein synthesis without affecting the gene expression.
Downregulation of CD20, a molecular target for monoclonal antibodies (mAbs), is a clinical problem leading to decreased efficacy of anti-CD20-based therapeutic regimens. The epigenetic modulation of CD20 coding gene (MS4A1) has been proposed as a mechanism for the reduced therapeutic efficacy of anti-CD20 antibodies and confirmed with nonselective histone deacetylase inhibitors (HDACis). Because the use of pan-HDACis is associated with substantial adverse effects, the identification of particular HDAC isoforms involved in CD20 regulation seems to be of paramount importance. In this study, we demonstrate for the first time the role of HDAC6 in the regulation of CD20 levels. We show that inhibition of HDAC6 activity significantly increases CD20 levels in established B-cell tumor cell lines and primary malignant cells. Using pharmacologic and genetic approaches, we confirm that HDAC6 inhibition augments in vitro efficacy of anti-CD20 mAbs and improves survival of mice treated with rituximab. Mechanistically, we demonstrate that HDAC6 influences synthesis of CD20 protein independently of the regulation of MS4A1 transcription. We further demonstrate that translation of CD20 mRNA is significantly enhanced after HDAC6 inhibition, as shown by the increase of CD20 mRNA within the polysomal fraction, indicating a new role of HDAC6 in the posttranscriptional mechanism of CD20 regulation. Collectively, our findings suggest HDAC6 inhibition is a rational therapeutic strategy to be implemented in combination therapies with anti-CD20 monoclonal antibodies and open up novel avenues for the clinical use of HDAC6 inhibitors.
Introduction
The clinical approval of anti-CD20 monoclonal antibodies (mAbs) in safe and effective therapeutic regimens has considerably changed the treatment paradigms in non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL). However, their efficacy in monotherapy is largely limited by the resistance mechanisms.1,2 Although anti-CD20 mAbs are incorporated into various chemotherapy-based combination regimens in all phases of conventional treatment,3 the overall response rates to this immunotherapy are still unsatisfactory.4,5 Poor response to anti-CD20 mAbs is especially pronounced in patients with CLL, in whom leukemic cells express low baseline levels of CD20 as compared with other B-cell malignancies.6,-8 Furthermore, in patients relapsing after initial treatment, development of resistance to anti-CD20 mAbs associated with a decrease in CD20 levels is commonly reported.9,,-12 An accumulating body of evidence suggests the level of CD20 on the surface of malignant B cells is a limiting factor determining the efficacy of anti-CD20 regimens.13,14 This especially holds true for rituximab and ofatumumab–type I mAbs that trigger activation of the complement cascade.
Until now, a number of factors regulating CD20 expression at both the transcriptional and posttranscriptional levels have been identified.8,15,,,,,-21 Among them, CD20 expression has been reported to be regulated epigenetically both by DNA methyltransferases22 and by histone deacetylases (HDACs).23 HDAC inhibitors (HDACis) are being explored in cancer research for their ability to restore the expression of silenced genes, and have recently emerged as highly effective treatments in combination with immunotherapies,24 including mAbs.25 The results presented so far revealed a therapeutic potential of nonselective pan-HDAC inhibitors increasing CD20 transcription (trichostatin A, valproic acid, romidepsin, and vorinostat [SAHA]) in combination with anti-CD20 mAbs.23,26,27 Recently, entinostat, a potent HDAC1 and HDAC3 inhibitor, has been demonstrated to enhance rituximab activity in preclinical studies by increasing survival rates by 30% in comparison with rituximab in monotherapy.28
HDACs are promising targets, particularly in hematologic malignancies.29,30 Four nonselective inhibitors have already been registered in monotherapies: romidepsin and SAHA for cutaneous T-cell lymphoma, belinostat for relapsed or refractory peripheral T-cell lymphoma, and panobinostat for multiple myeloma.31 These compounds, however, have been noted for their severe adverse effects, which can be burdensome in frail and heavily pretreated patients.32 It has been postulated that these toxicities could be avoided by the use of isoform-specific inhibitors,33,34 and thus various selective compounds are currently being tested in clinical trials. By now, HDAC6, an atypical member of HDAC family that regulates the acetylation status, and thus the activity of cytosolic proteins, has been explored therapeutically for its role in protein degradation. HDAC6 inhibition does not induce global changes in gene expression and cannot be truly considered an epigenetic modulator.35 It rather acts as a linker between ubiquitinated proteins and dynein, a motor protein that transfers misfolded protein cargo for disposal in aggresomes.36,37 HDAC6 also mediates the transport of the autophagic machinery to resorb protein aggregates and diminish their cytotoxicity.38 Thus, the disruption of the aggresome pathway, similarly to proteasome inhibition, results in a massive accumulation of misfolded protein aggregates and apoptotic cell death.39 As this strategy holds considerable potential in aggressive B-cell tumors with a high rate of protein synthesis, HDAC6 inhibitors ricolinostat (ACY1215) and ACY241 are currently being tested in phase 1 and 2 clinical trials in multiple myeloma (NCT01583283, NCT01997840, NCT02400242), non-Hodgkin lymphoma (NCT02091063), and CLL (NCT02787369). The results of preclinical studies show the increased efficacy of the combination of HDAC6 inhibitors with proteasome inhibitors in inducing stress-related cell death.40,-42 The preliminary outcomes of clinical trials show clinical benefit with mild to moderate adverse effects.43
The results of our research add a new intriguing observation to the current state of the art on HDAC6 function. We demonstrate that specific inhibition of HDAC6 isoform increases CD20 protein levels, which correlates with augmented sensitivity to anti-CD20 mAbs in vitro and in vivo. By using Click chemistry, we show that HDAC6 inhibition significantly increases synthesis of CD20 protein without affecting its total mRNA levels. Moreover, polysomal profiling reveals that HDAC6 inhibition increases the amount of CD20 mRNA associated with polysomes, which corresponds to actively translated fraction. Altogether, our results provide a well-evidenced rationale for the use of specific HDAC6 inhibitors as a strategy to sensitize B-cell malignancies to anti-CD20 therapy.
Materials and methods
Reagents
Rituximab was purchased from Roche, ofatumumab was a generous gift from Genmab A/S, and obinutuzumab was a generous gift from Roche Diagnostics. Trichostatin A (Sigma Aldrich), SAHA (Sigma Aldrich), scriptaid (Selleckchem), entinostat (Selleckchem), tubacin (Chemietek), tubastatin A (Sigma Aldrich), ricolinostat ACY1215 (Chemietek), homoharringtonine (Tocris), and Click-IT AHA (L-azidohomoalaine) (Thermo Scientific) were dissolved in dimethyl sulfoxide. Cycloheximide (Sigma Aldrich) was dissolved in water. Annexin V-fluorescein isothiocyanate (FITC) and propidium iodide (PI) were purchased from Sigma Aldrich.
Mice, tumor treatment, and monitoring
All in vivo experiments were performed on BALB/c severe combined immunodeficiency (SCID) females inoculated subcutaneously with 3×106 Raji cells. Rituximab (RTX)-treated mice were injected intraperitoneally with 10 mg/kg or 30 mg/kg RTX, ricolinostat-treated mice were injected intraperitoneally with 100 mg/kg ricolinostat (for details, see supplemental Methods, available on the Blood Web site). Treatment was performed 3 times per week for 3 consecutive weeks. Mice were euthanized when the tumor diameter reached 12 mm in at least 1 dimension.
Click-IT assays
To evaluate protein synthesis de novo, Click-IT AHA assays were performed according to the manufacturer’s protocol. Briefly, 4 × 106 Raji cells were co-incubated for 4 hours with 50 µM Click-IT AHA reagent and tested compounds (10 µM tubacin and translation inhibitors: 100 µg/mL cycloheximide and 1 µM homoharringtonine) in methionine-free medium. Afterward, the cells were washed twice with phosphate-buffered saline. For Alexa Fluor 488 staining of novel proteins, the cells were fixed with 3.7% paraformaldehyde, blocked with 3% bovine serum albumin, and permeabilized with 0.5% Triton-X. The cells were labeled with Click-IT reaction cocktail containing Alexa Fluor 488 azide and analyzed using flow cytometry. To assess the influence of tubacin on CD20 synthesis, the cells were lysed with 1% sodium dodecyl sulfate and labeled with biotin alkyne. The lysates were precipitated twice, using chloroform and methanol to eliminate unbound biotin particles. Biotin-labeled proteins were immunoprecipitated using Neutravidin Aggarose Resin (Thermo Scientific) and separated by sodium dodecyl sulfate/polyacrylamide gel electrophoresis. CD20 expression was subsequently assessed in biotinylated fraction by western blotting. β-actin level in input samples served as a loading control.
Isolation of polysomes and total cytoplasmic RNA
The procedure was essentially performed as described earlier.44 Briefly, cytosolic lysates from control and tubacin-pretreated (for 24 hours) Raji cells were prepared in lysis buffer (50 mM Tris-HCl at pH 7.4, 25 mM KCl, 5 mM MgCl2, 2 mM dithiothreitol, 250 mM sucrose, 0.7% Nonidet-P40, 100 µg/mL cycloheximide), using Dounce homogenizer, followed by 2 successive 10-min centrifugations at 4°C at 700g to pellet nuclei and 12 000g to pellet mitochondria. Then, the cytoplasmic fraction was divided in 2 portions. One portion containing 2 mg of cytosolic proteins was used as a source for total cytoplasmic RNA, using Trizol LS Reagent (Life Technologies) extraction protocol. The second portion containing 6 mg of cytosolic proteins was layered onto an 11-mL linear sucrose gradient (10%-40% sucrose supplemented with 50 mM Tris⋅HCl at pH 7.4, 25 mM KCl, 5 mM MgCl2, 10 mM dithiothreitol, and 100 µg/mL cycloheximide) and sedimented by a 2-hour centrifugation at 250 000g at 4°C in a SW41Ti rotor (Beckman). The gradients were collected in 15 fractions, and absorbance profiles were generated at 254 nm, using an ISCO UA-6 detector (Teledyne). Polysomal fractions were pooled for further RNA extraction using Trizol LS Reagent (Life Technologies).
Statistical analysis
Results were plotted with GraphPad Prism. Statistical significance was assessed by appropriate tests provided in figure legends. The P-values were marked with the asterisks on the charts (*P < .05, **P < .01, ***P < .001, ****P < .0001).
Results
HDAC6 isoform-specific inhibitors upregulate CD20 levels and increase the efficacy of anti-CD20 mAbs
Highly potent and selective HDAC6 inhibitors including tubacin, tubastatin A, and ricolinostat used at subcytotoxic concentrations (supplemental Figure 1A) significantly increased surface CD20 levels (Figure 1A), as well as the amount of CD20 protein in whole-cell lysates (Figure 1B) of Raji cells. The HDAC6 inhibition was confirmed by western blotting for acetylated tubulin (Figure 1B), a marker widely used for the inhibition of HDAC6 enzymatic activity. At the same time, the tested compounds did not affect the acetylation of histone H3 (supplemental Figure 1B), which is not a substrate for HDAC6. Importantly, all the tested inhibitors significantly increased the efficacy of both rituximab and ofatumumab in complement-dependent cytotoxicity (CDC) (Figure 1C). Because the efficacy of CDC also depends on the levels of membrane-bound complement regulatory proteins,14,45 we assessed CD46 and CD55 levels in Raji cells incubated with selected HDAC6 inhibitors. The levels of membrane-bound complement regulatory proteins underwent minor changes (supplemental Figure 2A), suggesting improved efficacy of rituximab and ofatumumab after pretreatment with HDAC6 inhibitors is a consequence of increased CD20 levels.
Specific HDAC6 inhibitors upregulate CD20 levels and potentiate the efficacy of anti-CD20 mAbs. (A-C) Raji cells were preincubated for 48 hours with increasing concentrations of HDAC6-specific inhibitors: tubacin, tubastatin A, and ricolinostat. (A) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of mean fluorescence intensity (MFI) of control cells (± standard deviation [SD]). Statistical significance was determined with Kruskal-Wallis test, **P < .01 vs controls. The experiments were repeated independently 3 times. (B) The levels of CD20 and acetylated-tubulin (a marker of HDAC6 inhibition) were assessed with western blotting in whole-cell lysates. β-actin was used as loading control. Densitometric analysis from 5 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± standard error of the mean [SEM]). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (C) Equal amounts of control and drug-pretreated cells were incubated for 60 minutes with rituximab (R-CDC) or ofatumumab (O-CDC; 1-100 µg/mL) and 10% human AB serum as a source of complement. Cell viability was assessed with PI staining. The survival of cells is presented as a percentage of control cells without antibody (± SD). Statistical significance was determined using 2-way analysis of variance test with Tukey’s correction, **P < .01, ***P < .001, ****P < .0001 vs controls. The experiments were repeated independently 3 times.
Specific HDAC6 inhibitors upregulate CD20 levels and potentiate the efficacy of anti-CD20 mAbs. (A-C) Raji cells were preincubated for 48 hours with increasing concentrations of HDAC6-specific inhibitors: tubacin, tubastatin A, and ricolinostat. (A) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of mean fluorescence intensity (MFI) of control cells (± standard deviation [SD]). Statistical significance was determined with Kruskal-Wallis test, **P < .01 vs controls. The experiments were repeated independently 3 times. (B) The levels of CD20 and acetylated-tubulin (a marker of HDAC6 inhibition) were assessed with western blotting in whole-cell lysates. β-actin was used as loading control. Densitometric analysis from 5 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± standard error of the mean [SEM]). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (C) Equal amounts of control and drug-pretreated cells were incubated for 60 minutes with rituximab (R-CDC) or ofatumumab (O-CDC; 1-100 µg/mL) and 10% human AB serum as a source of complement. Cell viability was assessed with PI staining. The survival of cells is presented as a percentage of control cells without antibody (± SD). Statistical significance was determined using 2-way analysis of variance test with Tukey’s correction, **P < .01, ***P < .001, ****P < .0001 vs controls. The experiments were repeated independently 3 times.
Antibody-dependent cell-mediated cytotoxicity contributes to the overall therapeutic efficacy of anti-CD20 mAbs. To evaluate the effects of HDAC6 inhibition on natural killer (NK) cell effector function, we used a model in which both target Raji cells and effector NK cells pretreated for 24 hours with selected HDAC6 inhibitors were co-incubated for 4 hours in the presence of HDAC6 inhibitors and rituximab. HDAC6 inhibition had no effect on either the efficacy of rituximab-mediated antibody-dependent cell-mediated cytotoxicity (supplemental Figure 2B) or degranulation of NK cells (supplemental Figure 2C). We observed that HDAC6 inhibitors potentiated cell death triggered by type II anti-CD20 mAb obinutuzumab (supplemental Figure 2D). Collectively, these results indicate HDAC6 inhibition may be an effective strategy in sensitizing tumor cells to anti-CD20 mAbs.
HDAC6 inhibition increases CD20 levels and potentiates the efficacy of anti-CD20 mAbs in a panel of tumor cell lines, in primary CLL cells and in vivo
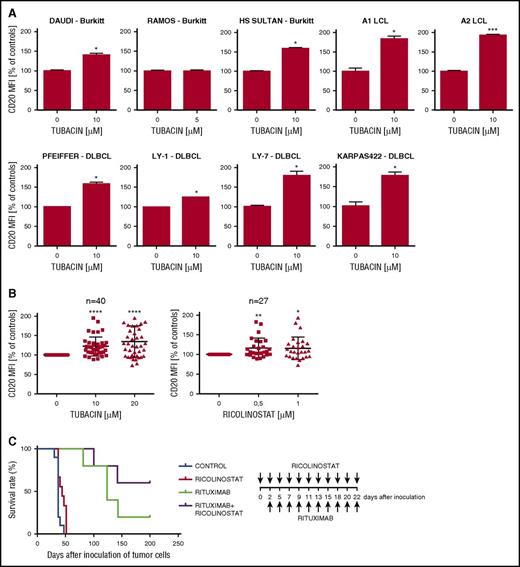
For further in vitro studies, tubacin, the first prototype chemical tool identified for HDAC6 with a higher specificity toward HDAC6 than other HDAC isoforms,35,46 was used as a model compound. In a panel of established Burkitt lymphoma and diffuse large B-cell lymphoma cell lines with various CD20 expression levels, as well as in Epstein-Barr virus (EBV)-infected lymphoblastoid cell lines, tubacin significantly upregulated CD20 (Figure 2A) and potentiated the efficacy of both rituximab and ofatumumab in CDC (supplemental Figure 3A). In a set of primary CLL samples with low baseline CD20 levels, both tubacin (n = 40) and ricolinostat (n = 27) significantly and dose-dependently increased surface CD20 levels (Figure 2B). Although the majority of primary cells isolated from patients were resistant to CDC, we observed a significant sensitization to ofatumumab-CDC after tubacin treatment (supplemental Figure 3B-C). Collectively, these data confirm that HDAC6 inhibition with small-molecule inhibitors upregulates CD20 expression in both established cell lines and primary cells, contributing to a significant increase of mAbs-mediated CDC. To determine whether the upregulation of CD20, resulting from HDAC6 inhibition, translates into improved antitumor efficacy of rituximab in vivo, we have treated SCID Fox Chase mice injected with Raji cells with clinically available ricolinostat. Although ricolinostat treatment alone did not influence the survival rate, it improved the overall survival of mice treated with rituximab (60% of cured mice) compared with rituximab-only-treated mice (20% of cured mice; Figure 2C), further confirming HDAC6 inhibitors improve the efficacy of anti-CD20 monoclonal antibodies.
HDAC6 inhibition increases CD20 levels in a panel of B-cell tumor cell lines, primary CLL cells and in vivo. (A) EBV-positive Burkitt lymphoma cell lines (Daudi, HS-Sultan), EBV-negative Burkitt lymphoma cell line Ramos, EBV-negative diffuse large B-cell lymphoma cell lines (Pfeiffer, Ly-1, Ly-7, Karpas 422), as well as EBV-transformed lymphoblastoid cell lines (A1, A2) were pretreated with 5 or 10 µM tubacin (depending on tubacin toxicity) for 48 hours. The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Mann-Whitney test, *P < .05, ***P < .001 vs control. The experiments were repeated independently twice. (B) Peripheral blood mononuclear cells from patients with CLL were treated with increasing concentrations of tubacin (n = 40) or ricolinostat (n = 27) for 48 hours. The cells were stained with anti-CD20-FITC, anti-CD19-phycoerythrin antibodies, and 7-aminoactinomycin D. Primary cells were gated according to side scatter and forward scatter, followed by doublet discrimination. CD20 expression was assessed in a population of CD19-positive, alive (7-aminoactinomycin D–negative) cells. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05, **P < .01, ****P < .0001, vs controls. (C) BALB/c SCID mice were inoculated subcutaneously with Raji cells stably transduced to express luciferase (Raji-LUC). Mice (n = 5-9) were then injected intraperitoneally with rituximab (10 mg/kg) and/or ricolinostat (100 mg/kg) 3 times a week for 3 consecutive weeks. Survival of mice was compared by Kaplan-Meier analysis. The experiment was performed once. Statistical significance was determined using log-rank survival analysis.
HDAC6 inhibition increases CD20 levels in a panel of B-cell tumor cell lines, primary CLL cells and in vivo. (A) EBV-positive Burkitt lymphoma cell lines (Daudi, HS-Sultan), EBV-negative Burkitt lymphoma cell line Ramos, EBV-negative diffuse large B-cell lymphoma cell lines (Pfeiffer, Ly-1, Ly-7, Karpas 422), as well as EBV-transformed lymphoblastoid cell lines (A1, A2) were pretreated with 5 or 10 µM tubacin (depending on tubacin toxicity) for 48 hours. The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Mann-Whitney test, *P < .05, ***P < .001 vs control. The experiments were repeated independently twice. (B) Peripheral blood mononuclear cells from patients with CLL were treated with increasing concentrations of tubacin (n = 40) or ricolinostat (n = 27) for 48 hours. The cells were stained with anti-CD20-FITC, anti-CD19-phycoerythrin antibodies, and 7-aminoactinomycin D. Primary cells were gated according to side scatter and forward scatter, followed by doublet discrimination. CD20 expression was assessed in a population of CD19-positive, alive (7-aminoactinomycin D–negative) cells. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05, **P < .01, ****P < .0001, vs controls. (C) BALB/c SCID mice were inoculated subcutaneously with Raji cells stably transduced to express luciferase (Raji-LUC). Mice (n = 5-9) were then injected intraperitoneally with rituximab (10 mg/kg) and/or ricolinostat (100 mg/kg) 3 times a week for 3 consecutive weeks. Survival of mice was compared by Kaplan-Meier analysis. The experiment was performed once. Statistical significance was determined using log-rank survival analysis.
The effect of HDAC6 inhibitors on CD20 levels is HDAC6-specific
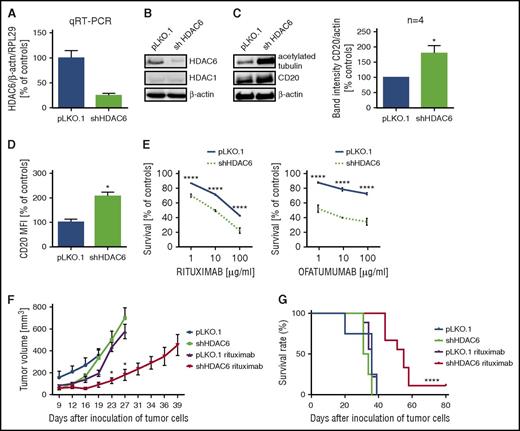
To investigate potential HDAC6-specific effects on CD20 levels, Raji cells were stably transduced with short hairpin RNA (shRNA) targeting HDAC6. Knock-down of HDAC6 was confirmed with quantitative reverse transcription polymerase chain reaction (qRT-PCR; Figure 3A) and western blotting (Figure 3B) and was associated with increased tubulin acetylation (Figure 3C) with no influence on the expression of another HDAC isoform (HDAC1) (Figure 3B). As a consequence of the specific HDAC6 knock-down, the expression of both total (Figure 3C) and surface (Figure 3D) CD20 protein in Raji cells increased. We observed the increased efficacy of rituximab- or ofatumumab-mediated CDC (Figure 3E) in cells with HDAC6 knock-down, despite increased surface levels of CD46 and CD55 complement regulatory proteins in these cells (supplemental Figure 4A). In contrast to tubacin, incubation of Raji cells with niltubacin, an inactive tubacin analog, had no effect on surface CD20 levels (supplemental Figure 4B). To further determine whether HDAC6 knock-down translates into improved antitumor efficacy of rituximab in vivo, we have used SCID Fox Chase mice inoculated subcutaneously with pLKO.1 Raji cells stably transduced with scrambled shRNA or pLKO.1-shHDAC6 Raji cells transduced with shRNA targeting HDAC6. Tumor growth in mice inoculated with pLKO.1-shHDAC6 Raji cells treated systemically with 30 mg/kg rituximab was significantly delayed when compared with control mice (Figure 3F). Importantly, on rituximab treatment, mice inoculated with pLKO.1-shHDAC6 Raji cells survived significantly longer than mice inoculated with control pLKO.1 Raji cells (median survival, 56 vs 36 days, respectively; Figure 3G). These results clearly indicate that upregulation of CD20 induced by HDAC6 inhibition plays an important role in regulation of antitumor activity of rituximab in vivo.
HDAC6 knock-down increases CD20 levels and potentiates the efficacy of rituximab in vitro and in vivo. Raji cells were stably transduced with either pLKO.1 or pLKO.1-shHDAC6. (A) HDAC6 levels were assessed with qRT-PCR with SYBRGreen. The experiments were repeated independently twice. (B) The levels of HDAC6 and HDAC1 were assessed in western blotting. β-actin levels were used as a loading control. The experiments were repeated independently twice. (C) The levels of CD20 and acetylated-tubulin were assessed in western blotting. β-actin level was used as a loading control. Densitometric analysis from 4 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs control. (D) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Mann-Whitney test, *P < .05 vs control. The experiments were repeated independently 3 times. (E) R-CDC and O-CDC were performed as described earlier (Figure 1D). Statistical significance was determined using 2-way analysis of variance test with Tukey’s correction, ****P < .0001 vs control. The experiments were repeated independently 3 times. (F-G) For in vivo studies, BALB/c SCID mice were inoculated subcutaneously with Raji cells either stably transduced with scrambled shRNA (pLKO.1) or shRNA against HDAC6 (pLKO.1-shHDAC6). Mice (n = 5-10) were then injected intraperitoneally with rituximab (30 mg/kg) 3 times a week for 3 consecutive weeks. (F) Effect of rituximab on tumor growth. Statistical significance was determined using multiple unpaired t tests, *P < .05, RTX pLKO.1 vs RTX shHDAC6. (G) Kaplan-Meier survival plot of mice pooled from 2 independent experiments. Statistical significance was determined using log-rank survival analysis, ****P < .0001, RTX pLKO.1 vs RTX shHDAC6.
HDAC6 knock-down increases CD20 levels and potentiates the efficacy of rituximab in vitro and in vivo. Raji cells were stably transduced with either pLKO.1 or pLKO.1-shHDAC6. (A) HDAC6 levels were assessed with qRT-PCR with SYBRGreen. The experiments were repeated independently twice. (B) The levels of HDAC6 and HDAC1 were assessed in western blotting. β-actin levels were used as a loading control. The experiments were repeated independently twice. (C) The levels of CD20 and acetylated-tubulin were assessed in western blotting. β-actin level was used as a loading control. Densitometric analysis from 4 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs control. (D) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Mann-Whitney test, *P < .05 vs control. The experiments were repeated independently 3 times. (E) R-CDC and O-CDC were performed as described earlier (Figure 1D). Statistical significance was determined using 2-way analysis of variance test with Tukey’s correction, ****P < .0001 vs control. The experiments were repeated independently 3 times. (F-G) For in vivo studies, BALB/c SCID mice were inoculated subcutaneously with Raji cells either stably transduced with scrambled shRNA (pLKO.1) or shRNA against HDAC6 (pLKO.1-shHDAC6). Mice (n = 5-10) were then injected intraperitoneally with rituximab (30 mg/kg) 3 times a week for 3 consecutive weeks. (F) Effect of rituximab on tumor growth. Statistical significance was determined using multiple unpaired t tests, *P < .05, RTX pLKO.1 vs RTX shHDAC6. (G) Kaplan-Meier survival plot of mice pooled from 2 independent experiments. Statistical significance was determined using log-rank survival analysis, ****P < .0001, RTX pLKO.1 vs RTX shHDAC6.
HDAC6 inhibition does not affect CD20 expression at a transcriptional level
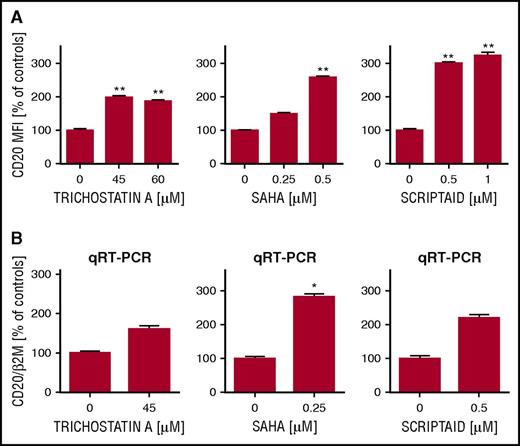
Previous studies reported that HDAC pan-inhibitors (trichostatin A, valproic acid, and romidepsin) increase CD20 levels.23,26 Accordingly, trichostatin A, scriptaid, and clinically available vorinostat, used in subcytotoxic concentrations, enhanced histone H3 acetylation (supplemental Figure 5A) and significantly increased CD20 at both protein (Figure 4A; supplemental Figure 5B) and mRNA (Figure 4B) levels, which corresponded to increased efficacy of rituximab in CDC (supplemental Figure 5C).
Pan-HDAC inhibitors upregulate CD20 levels. Raji cells were preincubated for 48 hours with increasing concentrations of pan-HDAC inhibitors trichostatin A, SAHA, and scriptaid. (A) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability and statistical analysis were performed as described earlier (Figure 1A). The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, **P < .01 vs controls. The experiments were repeated independently 3 times. (B) cDNA from Raji cells preincubated for 24 hours with HDAC pan-inhibitors was used for qRT-PCR amplification of CD20 and β2M with corresponding probes labeled with FAM and DABCYL. Relative reverse transcription quantitative polymerase chain reaction expression of CD20 gene was calculated by the user noninfluent second derivative method and shown as log-transformed target to reference ratio. B2M gene served as reference. The statistical significance was assessed using unmatched pairs t-test. *P < .05 vs controls. The experiments were repeated independently twice.
Pan-HDAC inhibitors upregulate CD20 levels. Raji cells were preincubated for 48 hours with increasing concentrations of pan-HDAC inhibitors trichostatin A, SAHA, and scriptaid. (A) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability and statistical analysis were performed as described earlier (Figure 1A). The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, **P < .01 vs controls. The experiments were repeated independently 3 times. (B) cDNA from Raji cells preincubated for 24 hours with HDAC pan-inhibitors was used for qRT-PCR amplification of CD20 and β2M with corresponding probes labeled with FAM and DABCYL. Relative reverse transcription quantitative polymerase chain reaction expression of CD20 gene was calculated by the user noninfluent second derivative method and shown as log-transformed target to reference ratio. B2M gene served as reference. The statistical significance was assessed using unmatched pairs t-test. *P < .05 vs controls. The experiments were repeated independently twice.
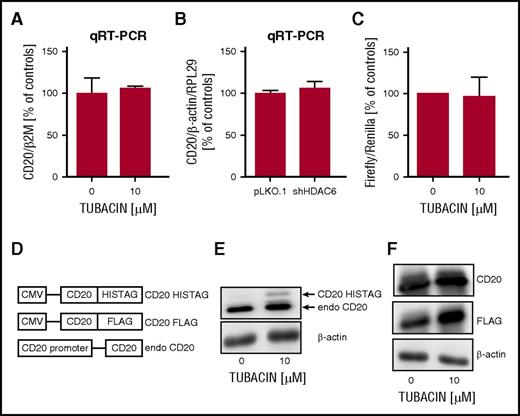
In contrast to HDAC pan-inhibitors, neither tubacin (Figure 5A) nor HDAC6 knock-down with shRNA (Figure 5B) affected MS4A1 transcription, as assessed in qRT-PCR experiments. To corroborate these findings, we tested the influence of tubacin on the activation of MS4A1 promoter. Correspondingly, in luciferase assay, tubacin did not change MS4A1 promoter activity (Figure 5C). Moreover, in Raji cells stably transduced with a vector encoding either His-tagged or FLAG-tagged CD20 fusion protein under CMV promoter (Figure 5D) and incubated with tubacin, we observed upregulation of the levels of both endogenous and exogenous CD20 proteins (Figure 5E-F). Altogether, these observations clearly demonstrate that the effects of HDAC6 inhibitors on CD20 levels are independent of the regulation of MS4A1 transcription and do not rely on the activity of MS4A1 promoter.
HDAC6 inhibition does not influence CD20 mRNA levels and MS4A1 promoter activity. (A) cDNA prepared from mRNA of Raji cells preincubated for 24 hours with 10 µM tubacin was used for qRT-PCR amplification of CD20 and β2M with corresponding probes labeled with FAM and DABCYL. (B) cDNA from Raji cells stably transduced with either pLKO.1 or pLKO.1-shHDAC6 was used for qRT-PCR using SYBRGreen. The experiments were repeated independently 3 times. (C) Relative luciferase activity was measured in lysates from Raji cells cotransfected with either empty vector or pGL4-wild-type CD20 promoter plus pRL-TK and incubated with 10 µM tubacin for a subsequent 24 hours. Statistical significance was determined with a Kruskal-Wallis test. The experiments were repeated independently 4 times. (D) A diagram illustrating plasmids used for modification of Raji cells. (E) Raji cells stably transduced with pLVX-CD20-HISTAG were incubated with 10 µM tubacin for 48 hours. The levels of endogenous CD20 and CD20-HISTAG were assessed with western blotting with anti-CD20 monoclonal antibody. (F) Raji cells stably transduced with pLVX-CD20-FLAG were incubated with 10 µM tubacin for 48 hours. The level of CD20-FLAG was assessed with western blotting with anti-FLAG antibody. The level of CD20 (both endogenous and exogenous) was assessed with anti-CD20 monoclonal antibody. β-actin level was used as loading control. The experiments were repeated independently twice.
HDAC6 inhibition does not influence CD20 mRNA levels and MS4A1 promoter activity. (A) cDNA prepared from mRNA of Raji cells preincubated for 24 hours with 10 µM tubacin was used for qRT-PCR amplification of CD20 and β2M with corresponding probes labeled with FAM and DABCYL. (B) cDNA from Raji cells stably transduced with either pLKO.1 or pLKO.1-shHDAC6 was used for qRT-PCR using SYBRGreen. The experiments were repeated independently 3 times. (C) Relative luciferase activity was measured in lysates from Raji cells cotransfected with either empty vector or pGL4-wild-type CD20 promoter plus pRL-TK and incubated with 10 µM tubacin for a subsequent 24 hours. Statistical significance was determined with a Kruskal-Wallis test. The experiments were repeated independently 4 times. (D) A diagram illustrating plasmids used for modification of Raji cells. (E) Raji cells stably transduced with pLVX-CD20-HISTAG were incubated with 10 µM tubacin for 48 hours. The levels of endogenous CD20 and CD20-HISTAG were assessed with western blotting with anti-CD20 monoclonal antibody. (F) Raji cells stably transduced with pLVX-CD20-FLAG were incubated with 10 µM tubacin for 48 hours. The level of CD20-FLAG was assessed with western blotting with anti-FLAG antibody. The level of CD20 (both endogenous and exogenous) was assessed with anti-CD20 monoclonal antibody. β-actin level was used as loading control. The experiments were repeated independently twice.
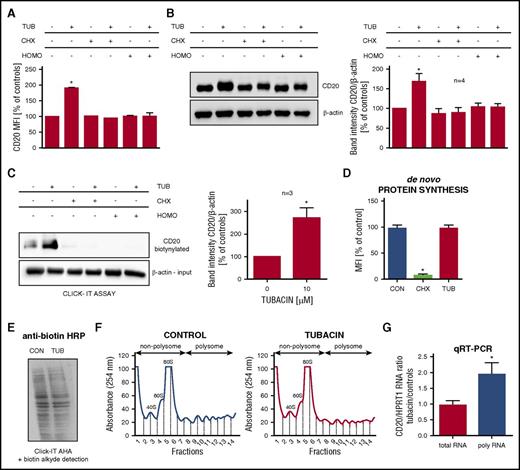
HDAC6 inhibition increases CD20 protein synthesis de novo through upregulation of CD20 mRNA translation
Because HDAC6 has been reported to be involved in degradation, endocytosis, and trafficking of intracellular vesicles, we sought to determine whether tubacin can regulate internalization of CD20 molecules using a reversible biotinylation assay. The analysis of the uncleaved, endocytosed biotin in this assay represents the amount of internalized CD20 in a time course. As presented in supplemental Figure 6A, CD20 undergoes a slow-rate endocytosis, which was further potentiated by tubacin. These results suggest the upregulation of CD20 by HDAC6 inhibition may not rely on the changes in CD20 endocytosis.
Next, to determine the half-life of CD20 protein in Raji cells, we blocked protein synthesis with cycloheximide and measured the decay of surface CD20 protein by flow cytometry (supplemental Figure 6B) and total CD20 protein by immunoblotting (supplemental Figure 6C). As a positive control, the stability of other proteins, namely, FOXO1, Mcl-1, and p53, was assessed. The steady state levels of these selected proteins declined significantly after a 24-hour incubation with cycloheximide (supplemental Figure 6D). Because no major differences were observed in CD20 levels between control and cycloheximide-treated cells during the 48-hour time frame, we assumed CD20 is essentially a very stable protein.
Given this slow turnover rate of CD20 protein, we conclude that the observed upregulation of its expression on HDAC6 inhibition in a 24-48-hour time frame may not be associated with changes in CD20 half-life. Moreover, we also observed that a 24-hour coincubation with translation inhibitors (cycloheximide and homoharringtonine) completely abolished the effects of tubacin on CD20 surface and total protein levels, as assessed with flow cytometry (Figure 6A) and western blotting (Figure 6B), suggesting the engagement of HDAC6 in the regulation of translation of CD20 mRNA.
HDAC6 inhibition increases CD20 synthesis de novo. (A) Raji cells were coincubated for 24 hours with 10 µM tubacin (TUB) and inhibitors of protein translation: 10 µg/mL cycloheximide (CHX) or 200 nM homoharringtonine (HOMO). The levels of surface CD20 were analyzed with flow cytometry as described in Figure 1A. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05 vs controls. The experiments were repeated independently 3 times. (B) Raji cells were coincubated with TUB, CHX, or HOMO as described in Figure 6A. CD20 levels in whole-cell lysates were assessed with western blotting. β-actin was used as loading control. Densitometric analysis from 4 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (C-D) Raji cells were coincubated for 4 hours with 50 µM Click-IT AHA and 10 µM tubacin and inhibitors of protein translation cycloheximide (100 µg/mL) or homoharringtonine (2 µM). (C) Newly synthesized proteins were labeled with biotin and immunoprecipitated using Neutravidin Aggarose beads. CD20 levels were assessed in biotinylated fraction, using western blotting. β-actin in input samples served as a loading control. Densitometric analysis from 3 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (D) Control, CHX, or tubacin-treated cells were analyzed with flow cytometry on staining of newly synthesized proteins with Alexa Fluor 488. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05 vs controls. The experiments were repeated independently twice. (E) Raji cells were coincubated for 4 hours with 50 µM Click-IT AHA and 10 µM tubacin. Newly synthesized proteins were labeled with biotin. Global de novo protein synthesis in control and tubacin-treated cells was assessed by western blotting with anti-biotin antibody. The experiments were repeated independently twice. (F-G) Control and tubacin-pretreated Raji cells were lysed in 25 mM KCl buffer, and the cytoplasmic fraction was separated onto a 10%-40% sucrose gradient. (F) Polysomal profiling of control and tubacin-treated cells. (G) Cytoplasmic RNA and polysomal-associated RNA from control or tubacin-pretreated Raji cells were reverse transcribed. CD20 levels were quantified by real-time polymerase chain reaction, using SYBR Green, and normalized to HPRT1 mRNA. qPCR analysis was performed in triplicates. Analysis of mRNA levels for each target was normalized to HPRT1 mRNA. The cytoplasmic RNA (totRNA) and the polysomal-associated RNA (polyRNA) ratios were determined as described in “Materials and methods.” The results are representative of the average RNA ratio ± SEM from 3 independent experiments. Statistical significance was determined with Kruskal-Wallis test, *P < .05 compared with total RNA.
HDAC6 inhibition increases CD20 synthesis de novo. (A) Raji cells were coincubated for 24 hours with 10 µM tubacin (TUB) and inhibitors of protein translation: 10 µg/mL cycloheximide (CHX) or 200 nM homoharringtonine (HOMO). The levels of surface CD20 were analyzed with flow cytometry as described in Figure 1A. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05 vs controls. The experiments were repeated independently 3 times. (B) Raji cells were coincubated with TUB, CHX, or HOMO as described in Figure 6A. CD20 levels in whole-cell lysates were assessed with western blotting. β-actin was used as loading control. Densitometric analysis from 4 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (C-D) Raji cells were coincubated for 4 hours with 50 µM Click-IT AHA and 10 µM tubacin and inhibitors of protein translation cycloheximide (100 µg/mL) or homoharringtonine (2 µM). (C) Newly synthesized proteins were labeled with biotin and immunoprecipitated using Neutravidin Aggarose beads. CD20 levels were assessed in biotinylated fraction, using western blotting. β-actin in input samples served as a loading control. Densitometric analysis from 3 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± SEM). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (D) Control, CHX, or tubacin-treated cells were analyzed with flow cytometry on staining of newly synthesized proteins with Alexa Fluor 488. The results are presented as a percentage of MFI of control cells (± SD). Statistical significance was determined with Kruskal-Wallis test, *P < .05 vs controls. The experiments were repeated independently twice. (E) Raji cells were coincubated for 4 hours with 50 µM Click-IT AHA and 10 µM tubacin. Newly synthesized proteins were labeled with biotin. Global de novo protein synthesis in control and tubacin-treated cells was assessed by western blotting with anti-biotin antibody. The experiments were repeated independently twice. (F-G) Control and tubacin-pretreated Raji cells were lysed in 25 mM KCl buffer, and the cytoplasmic fraction was separated onto a 10%-40% sucrose gradient. (F) Polysomal profiling of control and tubacin-treated cells. (G) Cytoplasmic RNA and polysomal-associated RNA from control or tubacin-pretreated Raji cells were reverse transcribed. CD20 levels were quantified by real-time polymerase chain reaction, using SYBR Green, and normalized to HPRT1 mRNA. qPCR analysis was performed in triplicates. Analysis of mRNA levels for each target was normalized to HPRT1 mRNA. The cytoplasmic RNA (totRNA) and the polysomal-associated RNA (polyRNA) ratios were determined as described in “Materials and methods.” The results are representative of the average RNA ratio ± SEM from 3 independent experiments. Statistical significance was determined with Kruskal-Wallis test, *P < .05 compared with total RNA.
To investigate the influence of tubacin on the specific translation of CD20, a metabolic labeling of nascent proteins with a methionine analog, Click-IT AHA (L-azidohomoalanine), was performed (supplemental Figure 8). Briefly, Raji cells labeled with Click-IT AHA were coincubated for 4 hours with tubacin or/and translation inhibitors followed by detection with alkyne-biotin. The level of CD20 protein in immunoprecipitated, biotin-labeled nascent protein fraction was determined with western blotting (Figure 6C). Tubacin strongly increased the levels of novel CD20 protein, whereas cycloheximide or homoharringtonine almost completely abolished CD20 synthesis de novo. Moreover, cytometric analyses, in which newly synthetized proteins were detected using Alexa Fluor 488 alkyne, confirmed that cycloheximide inhibited the overall level of protein translation (Figure 6D). Simultaneously, tubacin did not alter the overall levels of biotin-labeled nascent proteins in both flow cytometry (Figure 6D) and whole-cell lysate, as evaluated by western blotting (Figure 6E).
To substantiate our findings on increased translation of CD20 after HDAC6 inhibition, we performed polysomal profiling. Because translation is a cytoplasmic process, we analyzed the mRNAs isolated from the cytoplasmic cellular fraction. We first investigated whether tubacin influences global translation by comparing polysomal profiling curves. As shown in Figure 6F, there was no change in polysomal profiling curves between control and tubacin-pretreated cells, further confirming tubacin did not alter the overall protein translation. Importantly, our findings showed a significant increase in CD20 mRNA associated with polysomes in tubacin-treated cells (polyRNA Tub/Ctrl = 1.96) coupled with no significant changes in its total CD20 mRNA abundance (totRNA Tub/Ctrl = 0.97) (Figure 6G).
To clarify the mechanism of this regulation, we explored a widely known role of HDAC6 in translation and investigated the formation of stress granules (SGs), which might participate in accumulating and protecting RNA from harmful conditions. However, in both control and tubacin-treated Raji cells, we observed no SGs, suggesting HDAC6 is implicated in CD20 regulation independent of SGs (supplemental Figure 7). Together, our results clearly indicate HDAC6 is involved in a negative, post-transcriptional regulation of CD20 and that HDAC6 inhibition stimulates CD20 mRNA translation and further increases CD20 protein synthesis. However, the exact mechanisms of this regulation require further studies.
Discussion
HDAC6 inhibition has recently emerged as a promising therapeutic strategy for B-cell malignancies. On the basis of the results of in vitro cytotoxicity studies,42,47 HDAC6 inhibitors are currently being evaluated as monotherapy and in combinations in phase 1 and 2 clinical trials in patients with relapsed/refractory multiple myeloma and lymphoid malignancies. Since it has been shown that HDAC6 is overexpressed in primary human CLL cells,48 HDAC6 inhibitors are beginning to be explored in this malignancy. Recently, a phase 1 clinical trial of ricolinostat in combination with BCR inhibitors has been initiated in patients with relapsed or refractory CLL. Targeting HDAC6 in CLL has been further supported by recent in vitro data demonstrating decreased expression of immune checkpoint markers in CLL cells upon selective HDAC6 inhibition.49 Here, we identify a novel role of HDAC6 in B-cell malignancies that could be exploited therapeutically. The results of our studies clearly show that inhibition of HDAC6 significantly increases CD20 levels in a panel of established B-cell tumors and EBV-transformed lymphoblastoid cell lines, as well as in primary samples from patients with CLL. Although tubacin has been previously reported to act preferentially on EBV-positive Burkitt lymphoma cells,50 we observe that it significantly increases CD20 levels in both EBV-negative diffuse large B-cell lymphoma cell lines and in EBV-positive Burkitt lymphoma cells (Raji, Daudi, HS-Sultan), but not in EBV-negative Ramos cells. The observed upregulation translates into increased efficacy of anti-CD20 mAbs, particularly into inducing CDC, which is known to strongly rely on CD20 levels.13,51 Importantly, our observations are further confirmed by in vivo studies, in which we use complement-, NK cell- and macrophages-competent SCID mice, an optimal model for testing all mechanisms crucial for the efficacy of anti-CD20 monoclonal antibodies. We demonstrate that both pharmacologic and shRNA-mediated inhibition of HDAC6 activity significantly improves the survival of SCID mice treated with rituximab. Moreover, our in vitro results demonstrate that HDAC6 inhibition increases not only the efficacy of type I anti-CD20 mAbs but also enhances direct tumor cell death triggered by a novel type II anti-CD20 mAb, obinutuzumab.
The attempts to sensitize B-cell tumors to anti-CD20 mAbs have already been made mostly by using nonspecific pan-HDAC inhibitors.26 However, more specific HDACis, including entinostat, targeting HDAC1 and HDAC3, have been also reported to enhance the anti-tumor activity of rituximab.28 Interestingly, the authors did not observe increased efficacy of CDC, nor antibody-dependent cell-mediated cytotoxicity, in in vitro settings. The reported increase in both surface and total CD20 protein levels was significant but modest, suggesting another mechanism of this combination. In fact, entinostat seemed to potentiate rituximab-induced cell death by G1 cell cycle inhibition, p21 induction, and upregulation of adhesion molecules facilitating the interaction between tumor and immune cells.
The epigenetic modulation of CD20 coding gene has been proposed by others as a mechanism of CD20 upregulation by HDAC pan-inhibitors.23,26 However, HDAC6 is described as a unique member of HDAC family that does not affect chromatin organization. In this study, we employed highly selective HDAC6 inhibitors, such as tubacin, tubastatin A, and a currently clinically tested ricolinostat. We also confirmed our observations of HDAC6-specific effects on CD20 levels, using Raji cells stably transduced with shRNA targeting HDAC6.
To elucidate the mechanisms of the observed CD20 regulation, we performed a series of experiments assessing the influence of HDAC6 inhibition on CD20 transcription. We demonstrated that HDAC6 inhibition did not alter CD20 mRNA levels. Because HDAC6 has been mostly investigated for its effects on protein degradation, interactions with other proteins, or subcellular localization, we performed a reversible biotinylation assay to measure plasma membrane protein endocytic rates. So far, HDAC6 has been demonstrated to regulate EGFR52,-54 and CD13355 vesicular trafficking and degradation by controlling the acetylation status of α-tubulin and, subsequently, protein trafficking along microtubules. Here, we observed that CD20 underwent a slow-rate endocytosis that was slightly potentiated by tubacin, and therefore we also confirmed a previously described role of HDAC6 as a negative regulator of endocytosis associated with the endosomal compartments.
According to the cycloheximide chase assay, we concluded that CD20 is a protein with a long half-life of more than 48 hours, and thus rejected the hypothesis that HDAC6 is directly involved in CD20 degradation. Using several complementary methods, we demonstrated that HDAC6 regulates CD20 translation without changing the overall protein translation rate. Recently, modulation of mRNA translation has become an exciting area in the therapy of hematologic malignancies. It has been reported that translation downstream of BCR is differently regulated in CLL and normal B cells, which may provide an effective strategy for selective targeting of tumor cells.56
So far, the role of HDAC6 in protein translation was mainly described in the context of its participation in the formation of stress granules under stress conditions.57 Stress granules represent a complex assembly of proteins involved in the initiation and control of translation, as well as various polyadenylated mRNAs whose translation has been stalled. HDAC6 has been proposed as a central component regulating SG formation and potentially contributing to the control of RNA metabolism and translation. However, SGs are not are not detectable in Raji control cells or cells treated with tubacin (supplemental Figure 7). Thus, the observed increase in CD20 translation in tubacin-treated cells most probably does not result from the resumed translation of CD20 mRNA stalled in SG. Altogether we show that, in addition to the previously described role of HDAC6 in translation upon stress conditions, HDAC6 inhibition induces an increased translation of CD20 mRNA in Raji cells under normal conditions. However, the exact mechanism of this phenomenon requires further study. Because HDAC6 associates with the microtubule motor complex, and as local translation of mRNA occurs after transport via cytoskeletal motors, we propose that HDAC6 may negatively control translation of CD20 mRNA through spatiotemporal control of its translation.
To our knowledge, this is the first report showing that HDAC6 inhibition can be a therapeutic strategy successfully enhancing the efficacy of anti-CD20 mAbs. Our preclinical investigation might be relevant in terms of designing clinical studies and support further use of HDAC6 inhibitors in combination with anti-CD20 mAbs.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the patients involved in this study for their kind gift of samples.
The work was supported by National Science Center 2013/09/N/NZ3/01407 (M.B.), 2015/16/T/NZ6/00034 (M.B.), 2014/13/N/NZ6/02081 (M.S.), 2015/18/E/NZ6/00702 (M.W.), and 2013/11/B/NZ5/03240 (B.P.); European Commission 7th Framework Programme FP7-REGPOT-2012CT2012-316254-BASTION (J.G.); European Commission Horizon 2020 Programme 692180-STREAMH2020-TWINN-2015 (J.G.); Polish Ministry of Science and Higher Education grants IP2011 060271 (M.W.), DI2011 021241 (M.B.), DI 2014007344 (N.M.), and DI2013 006643 (A.D.); the Medical University of Warsaw grant 1M19/PM/112D/14/14 (M.B.); French Ministry of Research (E.B.); Ligue Nationale Contre le Cancer, Comité Départemental du Rhône (N.D.-V.); and Medical University of Lublin grant DS 462 (K.G.).
Authorship
Contribution: M.B., M.D., B.P., J.G., and M.W. performed and analyzed experiments and were involved in manuscript preparation; J.S., M. Kozikowski, M.S., N.M., P.Z., A.D., K.B., A.G.-J., M.G., A. Malinowska, A. Zerrouqi, and A. Zagozdzon performed experiments; J.S. and A. Muchowicz performed and analyzed in vivo experiments; isolation of polysomes was performed by E.B.; data obtained from polysomal profiles were analyzed by E.B., N.D.-V., and J.-J.D.; A. Malenda, M.K., J.B., D.G.E., L.L., D.B., L.F., E.L.-M., K.G., M. Slabicki, and T.Z. provided primary material and were involved in manuscript preparation; M.G., M.F., A. Zerrouqi, J.G., and M.W. provided expert advice and guidance throughout the study; and all authors reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Magdalena Winiarska, Department of Immunology, Medical University of Warsaw, Banacha 1 Str, Block F, 02-097 Warsaw, Poland; e-mail: magdalena.winiarska@wum.edu.pl; or Jakub Golab, Department of Immunology, Medical University of Warsaw, Banacha 1 Str, Block F, 02-097 Warsaw, Poland; e-mail: jakub.golab@wum.edu.pl.

![Figure 1. Specific HDAC6 inhibitors upregulate CD20 levels and potentiate the efficacy of anti-CD20 mAbs. (A-C) Raji cells were preincubated for 48 hours with increasing concentrations of HDAC6-specific inhibitors: tubacin, tubastatin A, and ricolinostat. (A) The levels of surface CD20 were analyzed with flow cytometry on staining with FITC-conjugated anti-CD20 antibody. Cell viability was assessed with PI staining. The results are presented as a percentage of mean fluorescence intensity (MFI) of control cells (± standard deviation [SD]). Statistical significance was determined with Kruskal-Wallis test, **P < .01 vs controls. The experiments were repeated independently 3 times. (B) The levels of CD20 and acetylated-tubulin (a marker of HDAC6 inhibition) were assessed with western blotting in whole-cell lysates. β-actin was used as loading control. Densitometric analysis from 5 independent immunoblots was performed using Image Studio Lite. The results are presented as a fold change of band intensities vs controls (± standard error of the mean [SEM]). Statistical significance was determined with Mann-Whitney test, *P < .05 vs controls. (C) Equal amounts of control and drug-pretreated cells were incubated for 60 minutes with rituximab (R-CDC) or ofatumumab (O-CDC; 1-100 µg/mL) and 10% human AB serum as a source of complement. Cell viability was assessed with PI staining. The survival of cells is presented as a percentage of control cells without antibody (± SD). Statistical significance was determined using 2-way analysis of variance test with Tukey’s correction, **P < .01, ***P < .001, ****P < .0001 vs controls. The experiments were repeated independently 3 times.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/14/10.1182_blood-2016-08-736066/4/m_blood736066f1.jpeg?Expires=1769080727&Signature=THm1qDbwQoOkL-QiMHUo0WtpoLcawGWxu3J~NvQ4L7VTmCHka~7XE-nFHpTXWBHFx0FmqBp6naxgxSz9EF2XLYMrqmmJdF1vZFEpWvf8sUpO6GAfVnJg70qySxXtXuNfK2bXog2I38MzIZeZFHrDtbotqDQdC--anZBPIkHDfXsowIpUWbIKlk9vOVJ1m~cs47x2CU79Wsaf3gjovN3Y4~WY8n~Z-fGdry3u7eTB6J~yF2JJCSzF03woIxrFNiz~WCKA-vlCrLY7gBaPG1rEVAaQbut6gLFlNGtmSy6iZwWc8pkAfLoqtCwdbPQRNvgwmIkskcN3dmw~tQ0~Y-WM~A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal