Abstract
Introduction
In Canada, Cyclophosphamide, bortezomib and dexamethasone (CyBorD) induction regimen has become the standard of care for transplant-eligible patients with newly diagnosed multiple myeloma (MM). In a phase II study, CyBorD produces a rapid and profound response without modifying the survival parameters (Leukemia . 2009 July; 23(7): 1337-1341). However, this protocol has never been compared to bortezomib and dexamethasone (Vel-Dex) regimen in a prospective trial. To compare the response at induction and at day-100 post autologous stem cell transplant (ASCT) and toxicity profiles of the Quebec population to these 2 regimens, we performed a retrospective trial in 2 tertiary centres in the Montreal area.
Objectives
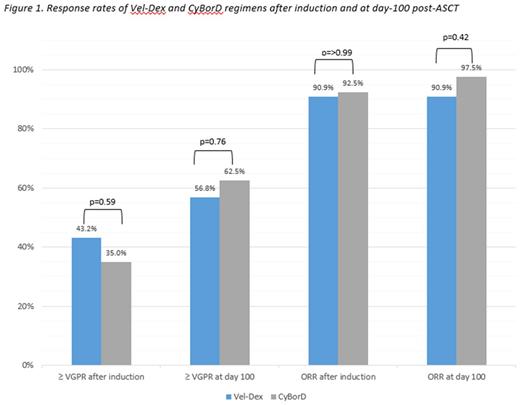
The primary objective was to compare overall response rates and very good partial responses or better (ORR and ≥ VGPR) between CyBorD and Vel-Dex after induction and at day 100 after ASCT. The secondary objectives were the evaluation of the toxicities and the overall survival at day 100 post-ASCT.
Method
We performed a retrospective observational multicenter study in a cohort of patients treated in Montreal area from January 1st 2010 to June 30th 2016. The inclusion criteria were patients ≥ 18 years-old with a new symptomatic MM diagnosis defined by the 2014 International Myeloma Working Group criteria, had received a first line induction treatment with Vel-Dex or CyBorD and were transplant eligible. Continuous variables were reported as a combination of means and medians and compared using Student's t-test and Mann-Whitney test respectively. Categorical variables were compared using Pearson's chi-square test.
Results
On a total of 99 patients, 84 were included and received CyBorD (n=40) or Vel-Dex (n=44) regimen. The median age was 56 and 59 years in CyBorD and Vel-Dex group respectively. Clinical characteristics were equivalent between the two groups, except for ISS stage III MM that were more numerous in Vel-Dex group (27.3% vs 17.5%; p=0.42) and MM with del17p ≥ 10% of alleles that were more frequent in CyBorD group (12.5% vs 3.4%; p=0.41). The mean cumulative bortezomib dose was 20.6 and 24.0 mg/m2 in Vel-Dex and CyBorD group respectively (p=0.002). There were no significant differences in term of modification in the regimen schedule. ORR and ≥ VGPR rates after a median of 4 cycles of induction were 92.5% and 35% for patients treated with CyBorD, and 90.9% and 43.2% for Vel-Dex respectively (p>0.99 and p=0.59). At day -100 post-ASCT, an ORR and ≥ VGPR rates of 97.5% and 62.5% for the CyBorD group and 90.9% and 56.8% for the Vel-Dex group, respectively (p=0.42 and 0.76) (Fig 1). No patient died within 100 days after ASCT. Also, there was no significant difference for the number of CD34 cells mobilized (15 in Vel-Dex vs 14.7x106/kg in CyBorD group; p=0.88). Treatment options after ASCT vary between the CyBorD and Vel-Dex groups for lenalidomide maintenance (10% vs 2%; p=0.3), second ASCT (2.5% vs 20.5%; p=0.02) and allogenic mini-transplant as part of a research protocol (10% vs 0%; p=0.05). Finally, there was not any evidence of a significant difference in terms of grade 3 and 4 toxicities, except for sensitive neuropathies that were more prevalent in the Vel-Dex group (15.9% vs 0%; p=0.01) even though the cumulative dose of bortezomib was significantly lower. However the very few toxicities noted prevent us from drawing any clear conclusion.
Conclusion
CyBorD and Vel-Dex appear to have similar overall efficacy for newly diagnosed transplant eligible patients with MM in our cohort.Surprisingly, the response at induction and at day-100 post-ASCT in the CyBorD group did not seem better nor deeper compared to the Vel-Dex group despite more stage III MM in the latter group. At day-100 post-ASCT, there may be a trend in favour of the CyBorD group, but the sample size is too small to detect a significant difference. Adding cyclophosphamide to the chemotherapy regimen did not seem to impair the stem cell collection and was not associated with more grade 3 or 4 toxicities. Longer follow-up is required to detect if what seems to be a more favourable response post-ASCT with CyBorD leads to differences in progression free survival and overall survival.
Adam: Novartis: Honoraria; Celgene: Honoraria; Gilead: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; Janssen: Honoraria; Apobiologix: Honoraria. Lemieux-Blanchard: Amgen: Honoraria; Takeda: Honoraria; Celgene: Honoraria; BMS: Research Funding; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal