Abstract
Introduction
Graft-versus-host disease (GVHD) remains a major problem after allogeneic-HCT as it is associated with high mortality, morbidity and poor quality of life. Rabbit anti-T cell globulin (ATG, Thymoglobulin) reduces GVHD without increasing relapse or mortality (Walker I: Lancet Oncol 2016). At multiple centers, including ours, ATG has become a standard component of conditioning. However, the efficacy of ATG is limited- at our center 40% patients still develop grade 2-4 aGVHD or moderate-severe cGVHD; 10% die of it and 25% survive with poor quality of life. We hypothesize that one of the reasons for the limited efficacy of ATG is suboptimal dosing (leading to low ATG levels in a fraction of recipients). Here we set out to determine the effect of pre- and post-HCT ATG exposure (area under the curve, AUC) on clinical outcomes and the factors influencing the AUCs in adult HCT recipients.
Methods
A total of 141 patients receiving first allo-HCT in Calgary with a peripheral blood stem cell graft after conditioning with fludarabine (250 mg/m2), busulfan (~12.8 mg/kg) +/- TBI (4 Gy) and GVHD prophylaxis with rabbit ATG (0.5 mg/kg on day -2, 2 mg/kg on day -1 and 2 mg/kg on day 0 before graft infusion), methotrexate and cyclosporine were included. Serum was collected at the end of the last ATG infusion, immediately pre-graft infusion, 30 minutes after the end of graft infusion and days 7, 14 and 28.
Serum levels of ATG capable of binding to lymphocytes were determined using a flow cytometric assay as previously described (Podgorny PJ: Biol Blood Marrow Transplant 2010). Pre-HCT ATG AUC was estimated from ATG levels at the end of the last ATG infusion and pre-graft infusion. Post-HCT ATG AUC was estimated from the ATG levels pre-graft infusion, 30 minutes post graft infusion and on days 7, 14 and 28. AUCs were split into terciles, quintiles and deciles for analysis.
Multivariate Cox regression was used to determine if ATG AUC was associated with mortality due to any cause or a composite outcome of death, relapse or moderate-severe chronic GVHD (the inverse of chronic GVHD relapse free survival, cGRFS). Multivariate competing risks regression was used to determine whether ATG AUC was associated with the cumulative incidence of cause-specific outcomes.
Results
Pre-/post-HCTAUC and Clinical Outcomes
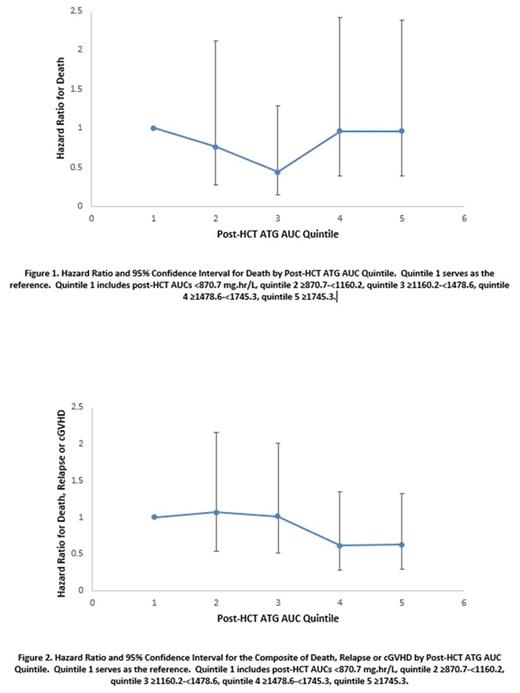
Intermediate post-HCT AUC appeared to be associated with lower mortality than low or high post-HCT AUC (Figure 1). This was significant when comparing the second tercile with the first tercile (HR=0.37, p=0.027) and the second with the third tercile (HR 0.38, p=0.032). However, high post-HCT AUC appeared associated with the lowest composite incidence of death, relapse or cGVHD (Figure 2). This was significant when comparing deciles 7-10 with deciles 1-6 (HR 0.60, p=0.047). The incidence of relapse was similar in all post-HCT AUC terciles/quintiles/deciles. As compared to deciles 1-6, deciles 7-10 were associated with a lower incidence of grade 2-4 aGVHD (HR 0.42, p=0.017) and moderate-severe cGVHD (HR 0.45, p=0.045), while GVHD-associated non-relapse mortality (NRM) (NRM preceded at any time by diagnosis of grade 2-4 aGVHD or moderate-severe cGVHD) trended towards a lower incidence (HR 0.28, p=0.097). Non-GVHD-associated NRM (NRM not preceded by diagnosis of grade 2-4 aGVHD or moderate-severe cGVHD) appeared to increase from the lowest to highest AUCs; however, there were too events for a meaningful statistical analysis.
Pre-transplant AUC did not appear to influence any of the above outcomes.
Factors influencing post-HCT AUC
Given that there appears to be an ideal (intermediate or high) post-HCT AUC and that low post-HCT AUC is deleterious, we next determined factors influencing the post-HCT AUC. The factors associated with (presumably influencing) the post-HCT AUC were body mass index (BMI) (Spearman correlation coefficient r = 0.24, p=0.005), day -2 (pre-ATG) blood lymphocyte count (r = -0.30, p<0.001) and possibly graft lymphocyte content (r = -0.14, p=0.081).
Conclusion
Low post-HCT ATG AUC is associated with the highest mortality and the highest composite of death, relapse or cGVHD. From the perspective of mortality, intermediate AUC may be ideal. In contrast, from the perspective of cGRFS, high AUC may be ideal. The post-HCT AUC appears influenced by BMI (when ATG is dosed per kg), pre-ATG blood lymphocyte count and graft lymphocyte content. We aim to develop a formula for ATG dosing that will avoid low post-HCT AUC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal