Abstract
BACKGROUND:
Venous thromboembolism (VTE) is a major cause of morbidity, and the second leading cause of mortality in cancer patients. VTE is associated with delay in cancer directed therapy, increased frequency and duration of hospitalization and overall healthcare costs. However, validated scoring systems for assessing risk of VTE are not widely used in clinical practice. We hypothesized that creation of a computerized risk calculator could help identify at-risk individuals in the ambulatory oncology setting; further, screening for VTE in high risk patients could lead to early detection of deep vein thrombosis (DVT) and avoid potential emergent consequences, including hospitalization.
METHODS:
A computerized alert was built into the electronic medical record system (EPIC) that automatically calculates a score using a validated risk tool [Khorana Score (KS), Blood 2008] based on the primary site of cancer, leukocyte and platelet counts, hemoglobin, and body mass index. During silent lead-in phase I (8/2016-1/17), we evaluated the accuracy of the electronic alert to detect high-risk patients and prospectively followed them for events. During this period, we limited the test to patients presenting to gastrointestinal, thoracic, genitourinary and lymphoma clinics. Patients presenting for consultation without planned treatment/follow up of at least 3 months at our institution were excluded. In phase II (6/17-12/17), we improved the electronic alert to warn physicians in real time about high risk patients and offered lower extremity ultrasonography as a screening test for early detection. In this phase, we only included patients with KS ≥ 3, and an available CBC <2 weeks from alert.
RESULTS:
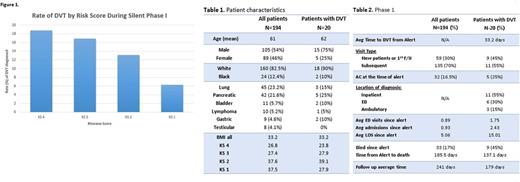
During phase I, the alert identified 194 consecutive patients as being at risk (see table 1). The majority of the patients with a positive alert were male (54%) with the most prevalent malignancy being lung and pancreatic adenocarcinomas. The subsequent rate of DVTs at 6 months in patients with a KS of 4 was 18.75% (3/17), patients with KS of 3 was 16.9% (11/65), KS of 2, 13.1% (8/61), and KS of 1, 6.25% (3/48) (Figure 1). See table 1.
Time from score calculation to DVT was an average of 33.2 days. 30% of patients developed a DVT within 4 weeks of alert, 50% within 60 days, and 65% within 90 days. 45% of patients diagnosed with DVT were alerted during their initial or second clinic visit. 55% of patients were diagnosed while inpatient and another 30% in the emergency room. Mean emergency room visits for patients with DVT were 1.75 compared to 0.89 for all patients. Mean all cause admissions and length of stay during this period were 2.43 and 15.01 days for patients with DVT, compared to 0.93 and 5.06 respectively for all 194 patients. Mortality rates were 45% for patients with DVT compared to 17% for the study population.
In phase II, 59 patients have been identified as high risk by the alert. Of these, 6 were already on therapeutic anticoagulation or had a recent history of DVT. Of the remainder, screening lower extremity ultrasonography was ordered on 10 patients; three (30%) had a LE DVT and were started on therapeutic anticoagulation. One other patient did not have screening ultrasonography ordered, and was diagnosed with DVT within 14 days and started on therapeutic anticoagulation. Additional data collection is ongoing and will be presented at the meeting.
CONCLUSION:
An electronic medical record risk calculator can be a valuable clinical tool in earlier detection of DVTs in high-risk cancer patients. An initial silent run-in phase demonstrates the ability of this tool to identify high-risk patients at substantially increased risk for VTE, emergency room visits, hospitalization and mortality. An ongoing phase II pilot of early screening demonstrates high rates of subclinical DVT but low rates of ordering screening tests by providers. Ongoing efforts to increase acceptance of screening ultrasonography and data collection may potentially reduce subsequent hospitalization and other adverse consequences for cancer patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal