Abstract
Introduction.During last years, a reduction in invasive aspergillosis (IA) incidence and mortality was observed in acute myeloid leukemia (AML) patients undergoing to induction phase of treatment. Instead, the incidence of IA and the attributable mortality rate (AMR) during the consolidation has not been recently evaluated. It is also uncertain whether posaconazole prophylaxis during induction chemotherapy affects IA on consolidation phase.
Design and Methods. The aim of our study was to evaluate incidence and mortality for IA in AML patients during the consolidation phase. All cases of proven/probable IA observed during consolidation chemotherapy in adult and pediatric patients with AML, who received conventional chemotherapy, between 2011 and 2015 were retrospectively collected in a multicenter study involving 38 Italian hematologic centers. All relevant clinical data were collected in CRFs.
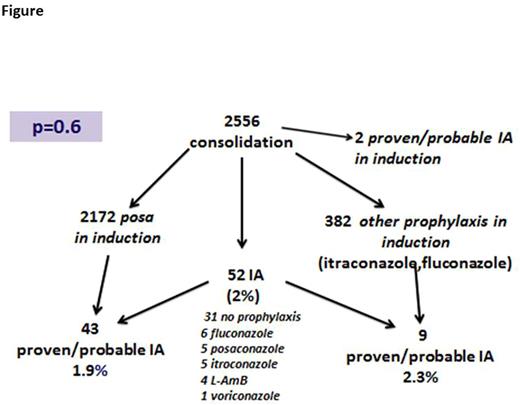
Results. A total of 2556 of AML patients in consolidation phase were registered. A total of 52 patients (2%) developed an IA [13 proven (0,5%) and 39 probable (1.5%)]. Male/female ratio was 33/19, median age was 57 yrs (range 5-79). As a consolidation, all these patients received high/intermediate doses cytarabine, in combination with an anthracycline in 30. Only 21 of 52 (40%) were on antifungal prophylaxis at the time of IA diagnosis: posaconazole in 5 (24%), fluconazole in 6 (28%), itraconazole in 5 (24%), liposomal amphotericin B (L-AmB) in 4 (19%) and voriconazole in 1 (5%). In 2 of 52 IA was a reactivation of an infection diagnosed during induction (Fig.).
Empiric antifungal therapy was initiated in 33 cases (65%) (mainly L-AmB: 24/33, 73%), while the remaining 19 (35%) received a pre-emptive/targeted approach. Fourteen cases switched from L-AmB to voriconazole, so that the most frequently targeted antifungal therapy was voriconazole (29/52, 55%). The median duration of antifungal treatment was 89 days (range 12-700). The overall mortality at day 120 was 19% (10/52), but the AMR was only 3.2% (5/52).
During induction, many patients (85%) received posaconazole as antifungal prophylaxis while the remaining 15% received other antifungals. (Fig.) During consolidation, antifungal prophylaxis was performed in about 50% of the patients. The most commonly used drug was fluconazole. In consideration of the hypothesized long-lasting activity of posaconazole, we also performed an analysis of incidence of IA during consolidation taking into whether or not the patients received posaconazole during induction. Considering the overall population of AMLs treated in consolidation no statistical differences were observed between those receiving in induction posaconazole or other prophylaxis, even if a lower percentage of patients in posaconazole arm developed an IA. (Fig.)
Conclusion. Our study shows that the incidence of IA during the consolidation in patients with AML is low but not absent. Similarly, also the AMR is low, likely due to advances in diagnosis and antifungal therapy. It is still a matter of discussion whether or not prophylaxis is needed in this subset of patients, since these are in remission and often candidates for transplantation. Finally, the long-lasting benefits of posaconazole is not confirmed but it might be correlated to the few cases of IA observed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal