Abstract
Hemophilia, or inherited genetic deficiencies in coagulation factors, results in uncontrolled bleeding requiring replacement therapy with recombinant proteins given preventively or on demand. However, a major problem with these approaches is the potential for development of immune responses to the administered proteins due to the underlying genetic deficiency of the factor(s) throughout life. As such, there is great interest in developing strategies that avoid immunogenicity and induce immune tolerance. Recently, recombinant factor VIII (rFVIII) and rFIX fused to the crystallizable fragment (Fc) domain of immunoglobulin G (IgG) have been developed as therapeutic agents for hemophilia A and B, respectively. Although it is well known that the possession of an Fc domain confers IgG’s longer-lasting circulating half-life, it is not generally appreciated that the Fc domain also confers immunoregulatory properties that are associated with the induction of tolerance. Here, we review some of the latest advances in our understanding of the tolerogenic abilities of IgG Fc and the impact of Fc-fusion proteins of rFVIII on the treatment of hemophilia.
Introduction
As a class of therapeutic moieties, crystallizable fragment (Fc)-fusion proteins have a long history of clinical use, dating back to 1998 when the first Fc-fusion protein product was approved for therapy.1 The rationale for such an approach stems from the ability of Fc-fusion proteins to confer the characteristics of both the immunoglobulin G (IgG) Fc domain and the chimerized protein or peptide. An important property of IgG is its long serum half-life due to interactions between the IgG Fc domain and neonatal Fc receptor (FcRn) conferring an extended half-life on the chimerized cargo drug.2-6 An underappreciated quality of Fc-fusion proteins is their ability to produce limited immunogenicity to the attached molecule. Indeed, several Fc-fusion drugs have been approved by the US Food and Drug Administration (FDA). Although there are no direct comparisons between the immunogenicity of the coupled (Fc-cargo) and uncoupled (cargo) therapies, it has been noted that the immunogenicity of such fusion proteins is low.1 The latter finding is consistent with observations dating back >40 years that IgG is endowed with tolerance-inducing functions that are conferred through the Fc domain.7-10
This is potentially important to recombinant replacement therapies whereby recurring supplementation of these compounds can trigger an immune-mediated reaction, as is the case for long-term treatment with recombinant factors VIII (rFVIII) and IX (rFIX) in humans with hemophilia A and hemophilia B, respectively, who are genetically or functionally deficient in these factors.11-13 Hence, administration of therapeutic factors VIII (FVIII) and IX (FIX) can result in the development of neutralizing anti-FVIII or anti-FIX IgG antibodies that can reduce the therapeutic effects of these proteins.14-18 Fc-fusion proteins of rFVIII (rFVIIIFc) and rFIX (rFIXFc) represent a new class of therapeutic proteins in which the Fc domain of human IgG1 is genetically fused to 1 molecule of rFVIII or rFIX, respectively, creating so-called monomeric Fc-fusion proteins that are produced in a human cell line that enables a human glycosylation pattern.19-23 As a consequence of these attributes, there is burgeoning evidence that FVIIIFc and FIXFc may be capable of being uniquely more effective in inducing antigen (Ag)-specific tolerance to these recombinant coagulation factors. Here, we summarize current evidence in support of this proposal, the potential mechanisms involved, and how these concepts may be used in current treatment regimens of hemophilia A and B for tolerance induction.
The relationship between IgG Fc and immune tolerance
In the late 1960s, Weigle and colleagues built on the newly discovered collaboration between T and B cells to examine mechanisms and targets for tolerance using ultracentrifuged human γ globulin (HGG) as a model Ag.24,25 They found that ultracentrifuged and deaggregated HGG was tolerogenic in mice, whereas aggregated HGG was immunogenic, suggesting tolerance was associated with monomeric IgG but not IgG as a complex. Furthermore, both T and B cells could be rendered unresponsive, but with different dose requirements and kinetics for tolerance induction and duration.
Yves Borel and coworkers subsequently expanded on these observations by demonstrating that direct coupling of immunogenic haptens (such as chemicals or nucleic acids) to murine IgG isotypes led to both T- and B-cell tolerance to the coupled epitopes and that IgG subclasses worked best as tolerogenic carriers relative to other proteins such as albumin or IgM.7-9,26-28 Baxevanis et al extended this work by examining the effect of coupling an Ag directly with human Fc.29 They found that human Fc could induce tolerance in mice, whereas a truncated Fc variant containing only the third constant heavy chain (CH3) domain could not. In addition, Waldschmidt and colleagues demonstrated in vitro that although intact IgG was a tolerogenic carrier, F(ab)′2 fragments were not, indicating the unique importance of the Fc domain of IgG for tolerance induction.10 Further studies by Scott’s group validated the use of IgG carriers and showed that potential immunogenic peptide epitopes could be rendered tolerogenic in an Ag-specific manner by genetically embedding them into an IgG framework.30-33
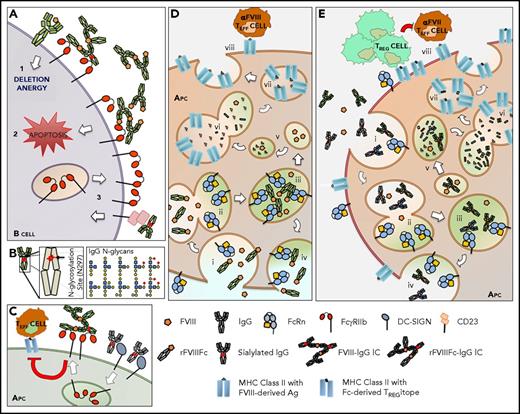
Although the mechanisms by which the IgG Fc domain can induce tolerance are poorly characterized, it has been suggested to involve FcR-dependent and independent interactions. In humans, 2 main classes of FcRs have been described and include the classical FcγRs (FcγR: FcγRI, FcγRIIa/b/c, FcγRIIIa/b), which are expressed primarily on the surface of hematopoietic cells, and nonclassical FcγRs (FcRn, dendritic cell [DC]–specific ICAM-3-grabbing nonintegrin [DC-SIGN], CD22, CD23, tripartite motif-containing 21 [TRIM21], Fc receptor like 1-6 [FcRL1-6], FCRLA, FCRLB), which have a broader cellular localization and cell-expression pattern (Table 1).34,35 Among the classical FcγRs, FcγRIIb is the sole receptor that possesses inhibitory function. It is also the only FcγR in mice and humans that is expressed on B cells although it is widely expressed on innate immune effector cells including monocytes, macrophages, and DCs and also on liver sinusoidal endothelium.36,37 In FcγRIIb-deficient mice, antibody production is strongly enhanced and less specific, resulting in autoantibody production and a systemic lupus erythematosus–like disease in susceptible mouse strains. Thus, IgG-Fc binding to FcγRIIb on B cells provides an important checkpoint for maintaining humoral tolerance and limiting self-reactive immune responses.38,39 Furthermore, Ag-antibody complexes (immune complexes [ICs]) may induce B-cell apoptosis by triggering FcγRIIb in the absence of B-cell receptor signaling, which may be an important mechanism to limit the survival of autoantibody-producing plasma cells in the bone marrow (Figure 1A).40-43
Human Fc receptors
| . | Classical FcγR . | Nonclassical FcR . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FcγRI . | FcγRIIa . | FcγRIIb . | FcγRIIc . | FcγRIIIa . | FcγRIIIb . | FcRn . | DC-SIGN . | CD22 . | CD23 . | TRIM21 . | FCRL1-6 . | FCRLA . | FCRLB . | |
| Other name | CD64 | CD32A | CD32B | CD32C | CD16A | CD16B | Brambell receptor | CD209; CLEC4L | SIGLEC2 | FcεRII | Ro52 | CD307a-f | ||
| Cellular distribution | Surface plasma membrane | Surface and endosomes | Surface plasma membrane | Surface | Cytoplasmic | Surface | Intracellular compartments | |||||||
| Functional outcome | Activation | Inhibition | Activation | IgG recycling; circulating immune complex responses | Ag presentation | Inhibition | Activation | Activation; viral degradation | Inhibition/ activation? | IgG retention during affinity maturation? | ||||
| Cellular expression | Hematopoietic | Most nucleated cells | Myeloid | B cells | Hematopoietic; epithelia | Most nucleated cells | Lymphocytes; mainly B cells | Germinal center B cells | ||||||
| Ig-binding affinity | IgG, high | IgG, low/medium | IgG, high; pH dependent | Sialylated IgG, medium | Sialylated glycans, surface IgM, CD45 | IgE, low | IgG, IgM, and IgA, medium | IgG aggregates, low/medium | IgG, low | |||||
| . | Classical FcγR . | Nonclassical FcR . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FcγRI . | FcγRIIa . | FcγRIIb . | FcγRIIc . | FcγRIIIa . | FcγRIIIb . | FcRn . | DC-SIGN . | CD22 . | CD23 . | TRIM21 . | FCRL1-6 . | FCRLA . | FCRLB . | |
| Other name | CD64 | CD32A | CD32B | CD32C | CD16A | CD16B | Brambell receptor | CD209; CLEC4L | SIGLEC2 | FcεRII | Ro52 | CD307a-f | ||
| Cellular distribution | Surface plasma membrane | Surface and endosomes | Surface plasma membrane | Surface | Cytoplasmic | Surface | Intracellular compartments | |||||||
| Functional outcome | Activation | Inhibition | Activation | IgG recycling; circulating immune complex responses | Ag presentation | Inhibition | Activation | Activation; viral degradation | Inhibition/ activation? | IgG retention during affinity maturation? | ||||
| Cellular expression | Hematopoietic | Most nucleated cells | Myeloid | B cells | Hematopoietic; epithelia | Most nucleated cells | Lymphocytes; mainly B cells | Germinal center B cells | ||||||
| Ig-binding affinity | IgG, high | IgG, low/medium | IgG, high; pH dependent | Sialylated IgG, medium | Sialylated glycans, surface IgM, CD45 | IgE, low | IgG, IgM, and IgA, medium | IgG aggregates, low/medium | IgG, low | |||||
A schematic representation of the potential mechanisms of tolerance induction by the Fc portion of IgG. (A) The ligation of the inhibitory receptor FcγRIIb by IgG IC (potentially composed of FVIII–anti-FVIII IgG or rFVIIIFc–anti-FVIII IgG) on B cells has different consequences depending on B-cell maturity and has been shown to (1) prevent B cells with a higher-affinity self-reactive receptor from becoming IgG+ plasma cells and (2) induce apoptosis. When sialylated IgG engages CD23, (3) B cells upregulate FcγRIIb expression. (B) In the CH2 domain of the IgG Fc region, a single conserved glycosylation site is located (asparagine, N297). This site hosts 2 sugar moieties per IgG with extensive heterogeneity due to the variable addition of fucose, galactose, bisecting N-acetylglucosamine, or sialic acid. These differences result in altered IgG binding to FcγRs, among others, which ultimately influences the effector functions of the Fc domain. For instance, (C) ligation of sialylated IgGs to DC-SIGN is involved in upregulation of inhibitory FcγRIIb on the surface of the APC, which modulates downstream APC functions. (D-E) Although APCs express FcRn on the surface, FcRn does not bind IgG at neutral pH. Thus, monomeric IgG or rFVIIIFc is internalized by (i) fluid-phase endocytosis and binds to FcRn in (ii-iii) an acidic endosomal compartment, the pH at which FcRn binds IgG. FcRn then recycles (iv) IgG or rFVIIIFc back into the neutral pH milieu of the circulation. FcRn unbound IgG or other internalized soluble proteins (FVIII) will be subsequently degraded in (v) lysosomes and routed to (vi-vii) Ag-processing compartments where loading onto MHC class II molecules takes place. Therefore, FcRn diverts IgG or recombinant protein fused to Fc from Ag presentation. (E) IgG not bound to FcRn due to levels that exceed FcRn capacity will also be degraded and peptides derived from IgG can be presented in the context of MHC class II molecules. (viii) Within the CH2 domain of Fc, tolerogenic epitopes are present and promote tolerance via TREG cell activation (Tregitope). As tolerance can be imposed upon proteins attached to Fc, these regulatory effects are likely to be transmissible. TEFF, T effector.
A schematic representation of the potential mechanisms of tolerance induction by the Fc portion of IgG. (A) The ligation of the inhibitory receptor FcγRIIb by IgG IC (potentially composed of FVIII–anti-FVIII IgG or rFVIIIFc–anti-FVIII IgG) on B cells has different consequences depending on B-cell maturity and has been shown to (1) prevent B cells with a higher-affinity self-reactive receptor from becoming IgG+ plasma cells and (2) induce apoptosis. When sialylated IgG engages CD23, (3) B cells upregulate FcγRIIb expression. (B) In the CH2 domain of the IgG Fc region, a single conserved glycosylation site is located (asparagine, N297). This site hosts 2 sugar moieties per IgG with extensive heterogeneity due to the variable addition of fucose, galactose, bisecting N-acetylglucosamine, or sialic acid. These differences result in altered IgG binding to FcγRs, among others, which ultimately influences the effector functions of the Fc domain. For instance, (C) ligation of sialylated IgGs to DC-SIGN is involved in upregulation of inhibitory FcγRIIb on the surface of the APC, which modulates downstream APC functions. (D-E) Although APCs express FcRn on the surface, FcRn does not bind IgG at neutral pH. Thus, monomeric IgG or rFVIIIFc is internalized by (i) fluid-phase endocytosis and binds to FcRn in (ii-iii) an acidic endosomal compartment, the pH at which FcRn binds IgG. FcRn then recycles (iv) IgG or rFVIIIFc back into the neutral pH milieu of the circulation. FcRn unbound IgG or other internalized soluble proteins (FVIII) will be subsequently degraded in (v) lysosomes and routed to (vi-vii) Ag-processing compartments where loading onto MHC class II molecules takes place. Therefore, FcRn diverts IgG or recombinant protein fused to Fc from Ag presentation. (E) IgG not bound to FcRn due to levels that exceed FcRn capacity will also be degraded and peptides derived from IgG can be presented in the context of MHC class II molecules. (viii) Within the CH2 domain of Fc, tolerogenic epitopes are present and promote tolerance via TREG cell activation (Tregitope). As tolerance can be imposed upon proteins attached to Fc, these regulatory effects are likely to be transmissible. TEFF, T effector.
The immune-modulating property of IgG is also dependent on glycosylation status. The Fc portion of IgG has a single carbohydrate modification site at an asparagine 297 residue that can produce at least 30 potential IgG glycoforms (Figure 1B) that have important consequences for the biologic activities and effector functions of antibodies.44 Ravetch and colleagues have shown that sialylated IgG glycoforms can bind DC-SIGN (or its mouse homolog SIGN-R1) and induce the expression of FcγRIIb by professional Ag-presenting cells (APCs), such as macrophages or DCs.45 These IgG glycoforms may promote tolerance presumably through suppression of APC function or promotion of Ag presentation of the internalized Ag in a tolerogenic fashion (Figure 1C).46 Furthermore, sialylated IgG glycovariants were demonstrated to upregulate the inhibitory FcγRIIb variant on human B cells in vitro and murine cells in vivo via binding to CD23, which limits antibody responses (Figure 1A).47 Thus, select IgG Fc glycoforms may be involved in limiting immune activation in both the adaptive humoral immune response and its downstream effector functions.
Among other nonclassical FcγR, FcRn is thought to mediate some of the tolerogenic properties of IgG. FcRn normally binds IgG through the CH2-CH3 domain of Fc at acidic pH as in an endosome of an APC, and protects it from degradation by diverting the IgG and its associated molecules away from lysosomes to the cell surface (Figure 1E).48 Thus, FcRn is not only responsible for the long serum half-life of IgG but is also a potential vehicle for preventing immunogenicity by diverting associated cargo, such as Fc fusion proteins, away from Ag-presentation compartments when the IgG is monomeric (Figure 1D).49-55 In addition, neonatal murine models of tolerance have demonstrated that maternally transferred IgG ICs can engage FcRn in mucosal DCs and induce FOXP3+ T regulatory (TReg) cells, thus linking FcRn to generation of tolerance pathways in certain settings.56
Finally, FcR-independent mechanisms include the observation that promiscuous tolerogenic epitopes may also exist in the CH2 domain of Fc, so-called “Tregitopes” proposed by DeGroot and colleagues.57 They have suggested that the Fc portion of IgG upon degradation is processed and presented by major histocompatibility complex (MHC) class II molecules that promote the activation of TReg cells (Figure 1E).57-59 Importantly, some of these Tregitopes overlap with regions critical for binding to FcγR and/or FcRn.57-62 On the other hand, additional studies have shown that some Tregitopes possess limited TReg cell triggering capacities consistent with the notion that the Fc portion of IgG engages multiple mechanisms of tolerance induction.63 Among the other potential mechanisms, it has been suggested that monomeric IgGs might negatively affect Ag uptake, processing, or loading onto MHC class II molecules by APCs rendering T-cell stimulation less efficient.64-66 Whether these mechanisms promote bystander tolerance to non-IgG epitopes attached to Fc remains to be determined.
Together, multiple mechanisms, both FcγR-dependent and -independent, potentially underlie the tolerance-inducing activities of IgG through its Fc domain and account in part for the anti-inflammatory activities of IV immunoglobulin.67
The relationship between IgG Fc and immune tolerance in models of hemophilia
Such concepts have direct potential relationship to the immunogenicity of, and immune tolerance to, FVIII and FIX. Building on these historical observations, the pioneering studies of Lei and Scott have shown that insertion of the immunogenic A2 and C2 FVIII domains into the Fc domain of IgG, creating chimeric IgG molecules, can preventatively induce FVIII-specific tolerance and actively induce tolerance in FVIII-immunized rodents.68 Notably, the latter observations represent more closely the clinical setting in that the inhibitors are present before the start of the therapy in most hemophilia A patients. Similarly, hemophilia A mice exposed to rFVIIIFc at therapeutically relevant doses (50 IU/kg and 100 IU/kg), but not higher doses (250 IU/kg), exhibit reduced antibody responses relative to that observed in response to rFVIII without an Fc domain.11 Moreover, pretreatment of hemophilia A mice with therapeutic doses of rFVIIIFc, but not an irrelevant protein, can prevent the induction of anti-FVIII antibodies including those with neutralizing potential. The mechanistic basis of the reduced immunogenicity of rFVIIIFc was found to involve a combination of immunomodulatory influences that are consistent with the induction of Ag-specific tolerance. Examination of splenocytes from rFVIIIFc-treated mice showed increased numbers of CD4+CD25+FOXP3+ TReg cells as well as an increase in T cells expressing the tolerogenic CD279 (PD-1) molecule.11 Further analysis of these splenic T cells revealed reduced expression of the proinflammatory protein tumor necrosis factor α and examination of their transcriptome confirmed increased expression of immunomodulatory molecules such as FOXP3, CTLA-4, interleukin-10, and transforming growth factor β. Furthermore, the levels of transcripts for proinflammatory molecules such as CCL3 and STAT3 were reduced in the spleens of rFVIIIFc-treated mice. Lastly, rFVIIIFc mutant molecules were generated that lacked the ability to bind to either FcγR or FcRn. In mice, the immunomodulatory influences of the 2 mutant forms of rFVIIIFc were maintained, although with a less-evident immune-regulatory profile as seen with the original rFVIIIFc protein. Overall, this murine study suggests that the immunomodulatory effect of rFVIIIFc is the combined result of increased numbers of TReg cells and the generation of a noninflammatory splenic microenvironment. There is also evidence that interaction with both FcRn and FcγR contributes to this outcome.
Among the FcγRs to be considered in the context of tolerance responses potentially associated with rFVIIIFc is the inhibitory FcγRIIb. FcγRIIb is a low-affinity IgG FcR that binds to ICs rather than monomeric IgG.69,70 As a consequence, rFVIIIFc is unlikely to bind FcγRIIb at therapeutic concentrations that typically achieve the levels of FVIII that normally exist in the circulation.20,22 As an IC, on the other hand, rFVIIIFc would be able to engage FcγRIIb and activating FcγR.71 It is thus interesting to consider the possibility that the presence of anti-FVIII or anti-rFVIIIFc antibodies might allow for formation of ICs capable of binding to and triggering FcγRIIb function, which might deliver inhibitory signals to B and other hematopoietic cells.43 However, FcγRIIb plays a complex role in regulating antibody-mediated tolerogenic pathways. This is illustrated by observations in a FVIII−/− mouse model where the presence of FcγRIIb was shown to be potentially detrimental in this regard through its ability to ensure survival of memory B cells during restimulation with FVIII.72,73 Therefore, in some instances, FcγRIIb may be necessary to protect memory B cells from overstimulation during FVIII reencounter and allow them to survive.
rFVIIIFc’s interaction with FcRn suggests that the molecule’s immunomodulatory effects might be transferred across the placenta as the FcRn is expressed by the syncytiotrophoblast and is involved in the transplacental transfer of IgG.74,75 This proposal is supported by evidence that an Fc fusion version of β-glucuronidase has been found to cross to the murine fetus.76 To date, preliminary evidence obtained in hemophilia A mice has also shown that when rFVIIIFc is administered at high doses to late-stage pregnant mothers, there is FVIII activity detectable in the fetus.77 This is not found in fetal mice treated with rFVIII only. Consistent with this, Gupta and colleagues12 have taken advantage of these concepts to further demonstrate the vital role played by FcRn in the transplacental transfer of IgG during gestation in relation to hemophilia.12,78 They have shown that the antenatal transfer of Fc containing the A2 and C2 domains of FVIII can induce FVIII-specific TReg cells in the progeny animals and prevent immune responses to rFVIII upon subsequent exposure during postnatal life.12 This is due to FVIII-specific tolerance induction as resistance to FVIII-associated immune responses can be transferred to previously naive animals. What is not known presently is how the transplacental transport of FVIII is influenced by its interaction with von Willebrand factor.77 Nevertheless, if this potential was realized, it might be possible to induce prenatal tolerance to FVIII, a significant step toward mitigating this treatment’s complication.
Mechanisms of immunogenicity of replacement clotting factors VIII and IX
As previously stated, the IV administration of therapeutic FVIII and FIX results in the development of neutralizing anti-FVIII or anti-FIX IgG, which are referred to as “inhibitors,” in up to 40% and 4%, respectively, of the patients with the severe forms of these diseases.16-18 Immune responses to FVIII and FIX are believed to be classical responses to foreign Ags: the proteins are endocytosed by professional APCs, processed, and presented to naive CD4+ T cells (Figure 1D); the naive T cells are activated, proliferate, and provide help to naive Ag-specific B cells that differentiate into plasmocytes or memory B cells. In the case of FVIII, the dependence on T-cell help was initially suggested in inhibitor-positive patients who became responsive to FVIII therapy following infection by HIV and loss of CD4+ T cells, as well as by the isotype-switched nature of anti-FVIII IgG (predominantly IgG1 or IgG4) and by the presence of affinity maturation.79-81 More directly, FVIII-specific CD4+ T cell lines or clones have been isolated from inhibitor-positive patients.82-84 Several factors have been proposed to predispose patients to FVIII inhibitor development. These include genetic risk factors, such as the type of hemophilia A–causing FVIII mutation, and more precisely, the presence of FVIII Ag, HLA-DR and DQ haplotypes, and polymorphisms in different immunoinflammatory genes (TNFA, IL10, HMOX1, FCGR).85-88 Other nongenetic risk factors have also been identified such as the type of FVIII product used, vaccination schedules, or the intensity of treatment in the first months of life.18,89
The nature of the immune regulation of the anti-FVIII response is poorly understood. Healthy donors can produce FVIII-reactive IgG and T cells, albeit under homeostatic conditions, suggesting that tolerance to FVIII relies on dynamic and controlled immune recognition rather than on the mere elimination of FVIII-specific T cells and B cells in primary lymphoid organs.90-92 Experiments in mice have suggested that induced tolerance to exogenous FVIII relies on the generation of both central (thymic) and peripheral (induced) TReg cells.12 Besides, the development of FVIII inhibitors was suggested to depend on an impaired capacity of the patients’ DCs to trigger indoleamine 2,3-dioxygenase 1 (IDO1)-dependent tolerance mechanisms.93 Yet, the facts that (i) healthy donors without previous abnormalities may develop pathogenic anti-FVIII autoimmunity (ie, acquired hemophilia) and (ii) patients with mild/moderate forms of the disease, who express mutated forms of the FVIII molecule, are at a lesser but life-long risk of developing FVIII inhibitors, illustrate the tenuous and complex nature of FVIII-specific regulatory mechanisms.94 Although less well understood, it is likely that similar mechanisms may underlie the hypersensitivity to FIX observed in patients with hemophilia B.95
Current treatment approaches and success rate for management of inhibitors
In some individuals with hemophilia who have low titer inhibitors (<5 Bethesda units [BU]/mL) to FVIII or FIX, higher doses of factor concentrate may be able to achieve hemostasis or even allow continued prophylactic therapy. However, for most patients with inhibitors, particularly those with high titers (>5 BU/mL), this precludes continued use of standard FVIII or FIX replacement therapy, making acute management of bleeding and prophylaxis more challenging. Thus “bypassing agents” have been the only available strategy to treat or prevent bleeding. The approved bypassing agents are an activated prothrombin complex concentrate (aPCC) or recombinant factor VIIa (rFVIIa).96 A recombinant porcine FVIII is approved for treatment of acute bleeding in patients with acquired hemophilia A, but is still being investigated in clinical trials in patients with congenital hemophilia A with inhibitors.97 Most recently, a humanized bispecific antibody, emicizumab, which partially mimics the scaffolding function of FVIII, has shown significant hemostatic activity in FVIII inhibitor patients and its properties were recently reviewed.98,99 This therapy has now been licensed for prophylactic management of bleeding in this patient population.
aPCC is a plasma-derived concentrate that contains both zymogen and active forms of vitamin K–dependent clotting factors, with its most important hemostatic components believed to be prothrombin and activated FX.98 The mechanism of action of rFVIIa is not entirely clear, however, evidence supports the notion that the therapeutic effect of high doses of rFVIIa in hemophilia stems from FVIIa-catalyzed activation of FX, requiring phospholipids exposed on activated platelets, but independent of tissue factor.96 Even though a scarce amount of information is available on their mode of action, both bypassing agents have demonstrated efficacy in achieving hemostasis with acute bleeding episodes of about 80%, with no clear evidence of superiority of either agent, although there is considerable interpatient and intrapatient variability.86 Thus, both agents may be used concomitantly. Clinical trials support the use of both bypassing agents for prophylaxis in hemophilia patients with inhibitors in association with reduction in the number of bleeding episodes and improvement in quality-of-life measures. However, overall efficacy in preventing bleeding episodes is inferior compared with prophylaxis in hemophilia patients without inhibitors and remains a substantial treatment burden that adds considerably to the overall costs of therapy. Thus, eradication of the inhibitor remains a high priority.
The standard of care for inhibitor eradication is thus immune tolerance induction (ITI). ITI therapy involves the frequent and regular infusion of FVIII or FIX, typically at high doses over months to years to induce tolerance to the infused factor and allow factor infusions alone to control acute bleeding and resumption of prophylaxis. The proposed mechanisms by which tolerance is induced have included T-cell exhaustion through overstimulation leading to T-cell anergy, inhibition of FVIII-specific memory B-cell differentiation, and the formation of anti-idiotypic antibodies.100-102
ITI is effective in about two-thirds of patients. However, observational studies have identified good- and poor-risk features that affect successful outcome. Poor-risk features include age at start of ITI of >8 years old, a historical peak titer of >200 BU/mL, pre-ITI titer of >10 BU/mL, and time to titer decline to <10 BU/mL before ITI of >24 months, with tolerance success rates that are <50%. The International Immune Tolerance Study demonstrated an overall success rate of ∼70% in subjects with good-risk features.103 This study was a randomized, controlled study comparing low-dose (50 IU/kg 3 times per week) to high-dose FVIII (200 IU/kg daily) and did not show a significant difference between the dosing regimens in overall tolerance induction success rate. However, high-dose subjects achieved a negative titer and recovered significantly more rapidly than low-dose subjects (4.2 months vs 9.2 months). In addition, there was a significantly greater number of bleeding episodes in the low-dose subjects. ITI has significant financial implications, with costs of approximately $50 000 to $75 000 per month not including the high cost associated with the chronic use of bypassing agents. Economic modeling has suggested that low-dose ITI combined with aPCC prophylaxis could be a cost-saving strategy with the potential to reduce the morbidity by lowering the risk of breakthrough bleeding during ITI.104 These observations highlight the critical need for additional approaches to prevent and manage the complication of inhibitor formation.
Potential immunomodulatory properties of rFVIIIFc and rFIXFc in the management of inhibitors
The immunomodulatory properties of rFVIIIFc have suggested that it may be beneficial to hemophilia patients in preventing inhibitor formation or in those in whom inhibitors have already developed. There are now several pieces of clinical evidence that support this proposal.
rFVIIIFc and rFIXFc display extended stability and availability in the circulation, through interaction of the IgG-Fc domain with FcRn, diverting the chimeric proteins away from intracellular degradation, although this half-life extension is greater with FIX than FVIII due to the latter’s interaction with von Willebrand factor.105-107 Importantly, passage of rFVIIIFc through intracellular recycling routes does not affect its overall function, and studies involving FVIII (rFVIII-SQ) stability at different pH levels have shown that its activity is minimally lost at pH 6.20,22,108,109 It was only below this pH level that FVIII activity was increasingly absent.108 Furthermore, the endocytic recycling pathway where FcRn operates to salvage IgG from lysosomal degradation involves mildly acidic environments characteristic of an early endosome, sorting endosome, and recycling endosome where the lowest pH is between ∼5.8 and 6.5.49,110-113 In this mildly acidic environment, the activity of FVIII would thus be expected to be preserved. Consequently, both rFVIIIFc and rFIXFc have demonstrated efficacy in managing acute bleeding episodes and in preventing bleeding through prophylaxis.114,115 In addition, to date, no inhibitors have been reported within previously treated patient populations with either Fc fusion product. There is thus good biological rationale for reduced immunogenicity of these fusion proteins as well as improved efficacy in ITI based upon the aforementioned comments, recognizing, however, that this requires additional studies in controlled ITI trials and in previously untreated patient populations. Moreover, recent clinical data support this notion.13,116 However, definitive confirmation in this regard awaits clinical data from previously untreated patients and in prospective ITI studies.
In a case report for example, Ragni and colleagues noted that in comparison with a child in an inhibitor-prone family who developed a high-titer inhibitor in response to conventional rFVIII treatment, a cousin with severe hemophilia A was observed to develop low-titer inhibitors when treated with rFVIIIFc.116 Furthermore, the child who received rFVIIIFc was able to continue prophylactic dosing with rFVIIIFc with subsequent resolution of the inhibitor, whereas the rFVIII-only family member went on to require placement of a port central venous catheter and high-dose ITI to eradicate the inhibitor.116 In addition, 2 case series have described the successful induction of FVIII tolerance in 4 children with severe hemophilia A and high-titer inhibitors using doses of rFVIIIFc ranging from 50 IU/kg 3 times per week up to 200 IU/kg every other day.13,117 In a report from Malec and colleagues,117 the time to disappearance of anti-FVIII antibodies was 4 to 12 weeks, which was shorter than that reported with rFVIII ITI. More recently, a noninterventional, retrospective chart review of males with severe hemophilia A and high-titer inhibitors treated with rFVIIIFc for ITI was conducted at 10 sites in the United States and Canada.118 Nineteen patients were treated: 7 first-time ITI and 12 who had previously failed ITI with other products (rescue ITI). Although this retrospective study included a patient population with poor-risk features for ITI success, rFVIIIFc use demonstrated a rapid decrease in BU titers and rapid tolerization in first-time ITI patients, and showed therapeutic benefit in patients undergoing rescue ITI. Furthermore, a trend toward rapid BU titer decline was observed with higher rFVIIIFc dosing (>130 IU/kg) administered daily. These preliminary results will be evaluated further in 2 prospective clinical trials using rFVIIIFc for ITI in patients with hemophilia A and inhibitors (NCT03093480 and NCT03103542) to determine whether an immunomodulatory influence of rFVIIIFc may be more prompt and efficient than current ITI protocols. In addition, a phase 2 clinical study has been organized to assess the influence of rFVIIIFc on inhibitor incidence in previously untreated patients (the INHIBIT study; clinicaltrials.gov identifier NCT02196207).119 Confirmation of the immunomodulatory influence of rFVIIIFc in enhancing the efficiency of current ITI protocols will require the design of appropriate clinical trials that are now ongoing. Similar studies should be considered for patients with hemophilia B in light of a case report describing the successful use of rFIXFc in an extended infusion protocol to treat a patient with a history of hypersensitivity to plasma-derived and other rFIX products.120 Notwithstanding this initial report, more clinical data need to be collected to confirm the immunomodulatory potential of rFIXFc.
Concluding remarks
FVIII and FIX are highly immunogenic proteins when used as long-term replacement therapy in patients with hemophilia A and B, respectively. This fact significantly complicates the management of these diseases. These immune responses represent a major burden on patients and the health care system, necessitating a better understanding of the pathways involved in the pathogenic immune responses, their regulation, and novel means to mitigate the complication through the induction of immune tolerance. The development of rFVIII and rFIX as fusion proteins with the Fc domain of IgG1 for the treatment of these patients is increasingly recognized to provide a unique opportunity for confronting this problem. The possession of an IgG Fc domain not only endows FVIII and FIX with extended pharmacokinetic survival due to interactions with FcRn, but also potentially takes advantage of the less-appreciated but equally important property of the Fc domain as a factor involved in tolerance induction as reviewed here. Indeed, the recent application of rFVIIIFc and rFIXFc to humans with hemophilia A and B has revealed encouraging evidence that coupling these proteins to Fc may, at present mainly with rFVIIIFc, alter the host immune response in a manner that is associated with enhanced tolerance induction. These timely observations raise the possibility that such fusion proteins may be less immunogenic and/or allow for enhanced induction of factor-specific tolerance relative to their native counterparts, which will require ongoing and newly established protocols focused on addressing the major clinical challenges associated with coagulation factor immunogenicity. It is hoped that this review article will stimulate such preclinical and clinical studies and the opportunities that they provide.
Acknowledgments
D.L. was supported by a Canada Research Chair in Molecular Hemostasis and by Canadian Institutes of Health Research (CIHR) Foundation grant FDN-154285. S.W.P. was supported by research grants from Shire and the Goerlich Foundation. S.L.-D. was supported by INSERM, Centre National de la Recherche Scientifique (CNRS), Université Pierre et Marie Curie (UPMC) Paris 6, and a grant from Agence Nationale de la Recherche (ANR-10-BLAN-1118). M.P. was supported by CIHR. F.N. was supported by grants from the German Research Foundation (CRC1181-A7, GK1660, TRR130-P13), the Interdisziplinäre Zentrum für Klinische Forschung (IZKF) Erlangen (A68), and the Emerging Fields Initiative. D.W.S. was supported by National Institutes of Health (NIH) National Heart, Lung, and Blood Institute grants HL126727 and HL127495. R.S.B. was supported by NIH National Institute of Diabetes and Digestive and Kidney Diseases grant DK053056 and NIH Harvard Digestive Disease Center (HDDC) grant P30 DK034854.
Authorship
Contribution: D.L., S.W.P., S.L.-D., M.P., F.N., D.W.S., and R.S.B. prepared, edited, and approved the manuscript.
Conflict-of-interest disclosure: D.L. receives research support from Bioverativ, Bayer, CSL-Behring and Octapharma. S.W.P. serves as a consultant to Bioverativ, Shire, Novo Nordisk, Pfizer, and CSL Behring. S.L.-D. serves as a consultant for SOBI. F.N. served as a consultant to SOBI. R.S.B. serves as a consultant to Bioverativ. The remaining authors declare no competing financial interests.
A complete list of the IgG Fc Immune Tolerance Group collaborators appears in “Appendix.”
Correspondence: Richard S. Blumberg, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, New Research Building, Room 641b, 77 Ave Louis Pasteur, Boston, MA 02115; e-mail: rblumberg@bwh.harvard.edu; and David Lillicrap, Department of Pathology and Molecular Medicine, Queen’s University, Richardson Laboratory, 88 Stuart St, Kingston, ON K7L 3N6, Canada; e-mail: dpl@queensu.ca.
Appendix: group collaborators
The members of the IgG Fc Immune Tolerance Group collaborators are: Steven W. Pipe (Department of Pediatrics and Pathology, University of Michigan, Ann Arbor, MI), Sebastien Lacroix-Desmazes (Sorbonne Universités, Université Pierre et Marie Curie-Paris 06, INSERM, Université Paris Descartes, Sorbonne Paris Cité, Unité Mixte de Recherche [UMR] S 1138, Centre de Recherche des Cordeliers, Paris, France), Michal Pyzik (Division of Gastroenterology, Hepatology, and Endoscopy, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA), Falk Nimmerjahn (Institute of Genetics, Department of Biology, University of Erlangen-Nuremberg, Erlangen, Germany; Medical Immunology Campus Erlangen, Department of Biology, University of Erlangen-Nuremberg, Erlangen, Germany), and David W. Scott (Department of Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal