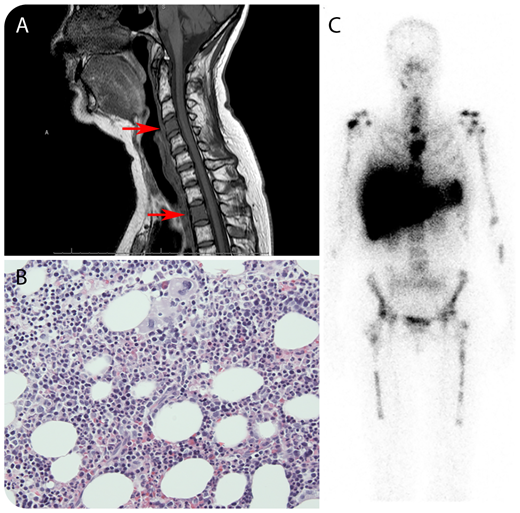
A 47-year-old woman presented with complaints of severe, persistent neck pain, 7 years after treatment of severe aplastic anemia with immunosuppression (antithymocyte globulin, methylprednisolone, and cyclosporine). A complete remission was achieved 5 months after this treatment. When her complaints were analyzed with a magnetic resonance imaging (MRI) scan of the cervical spine, an image suspicious for metastases in several vertebral corpora was found (panel A, MRI of the cervical spine; arrows indicate aberrant signals of the corpus of cervical vertebra 4 and thoracic vertebra 2). An 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) computed tomography (CT) scan revealed FDG-avid lesions throughout the axial spine, sternum, sacrum, femurs, and both mammae. Biopsies were taken from the mammary lesions, showing no malignancy. Subsequently, biopsies were taken from the right femur and sacrum, showing normal hematopoiesis without suspicion for malignancy (panel B; original magnification ×20, hematoxylin and eosin stain). Next, bone-marrow (BM) scintigraphy (99mTc-nanocolloid) was performed, confirming focal spots of increased BM activity in the suspected lesions (panel C). Here, increased and patchy BM activity may have been caused by patchy BM reconstitution in response to treatment in the setting of aplastic anemia. On MRI or 18F-FDG-PET/CT scan, increased BM activity may mimic malignant disease. BM scintigraphy using 99mTc-nanocolloid is preferred over 18F-FDG-PET or 18F-fluorothymidine–PET scan to demonstrate this, because it differentiates between hematopoiesis and other tissues.
Clinically, the neck pain resolved spontaneously and was probably unrelated to BM activity because the patient had no pain at other involved sites.
A 47-year-old woman presented with complaints of severe, persistent neck pain, 7 years after treatment of severe aplastic anemia with immunosuppression (antithymocyte globulin, methylprednisolone, and cyclosporine). A complete remission was achieved 5 months after this treatment. When her complaints were analyzed with a magnetic resonance imaging (MRI) scan of the cervical spine, an image suspicious for metastases in several vertebral corpora was found (panel A, MRI of the cervical spine; arrows indicate aberrant signals of the corpus of cervical vertebra 4 and thoracic vertebra 2). An 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) computed tomography (CT) scan revealed FDG-avid lesions throughout the axial spine, sternum, sacrum, femurs, and both mammae. Biopsies were taken from the mammary lesions, showing no malignancy. Subsequently, biopsies were taken from the right femur and sacrum, showing normal hematopoiesis without suspicion for malignancy (panel B; original magnification ×20, hematoxylin and eosin stain). Next, bone-marrow (BM) scintigraphy (99mTc-nanocolloid) was performed, confirming focal spots of increased BM activity in the suspected lesions (panel C). Here, increased and patchy BM activity may have been caused by patchy BM reconstitution in response to treatment in the setting of aplastic anemia. On MRI or 18F-FDG-PET/CT scan, increased BM activity may mimic malignant disease. BM scintigraphy using 99mTc-nanocolloid is preferred over 18F-FDG-PET or 18F-fluorothymidine–PET scan to demonstrate this, because it differentiates between hematopoiesis and other tissues.
Clinically, the neck pain resolved spontaneously and was probably unrelated to BM activity because the patient had no pain at other involved sites.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal