Abstract
Background: Readmissions within 30 days after index hospitalization is a quality, and cost-containment metric. It is now a major issue for hospitals, physicians and policy makers. Financial penalties to hospitals with high rates of risk adjusted readmissions have been expanded beyond medical conditions like heart failure and pneumonia. Auto-HCT is a widely used therapeutic strategy in the management of various hematological disorders, particularly multiple myeloma (MM) and non-Hodgkin lymphoma (NHL) in the US. However, auto-HCT readmission rates are poorly described in the literature and often limited to single center studies. To better address the incidence and underlying predictors of 30-day readmission following auto-HCT, we performed an analysis of the Nationwide Readmission Database(NRD).
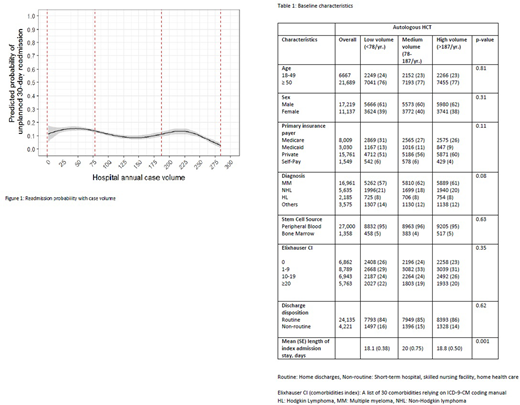
Methods: NRD data was queried from 2012-2014 to identify patients >18 years of age discharged from the hospital after auto-HCT (identified as presence of any ICD-9 procedure codes 41.00, 41.01, 41.04, 41.07, or 41.09). Survey weighted domain analysis was conducted to study incidence of 30-day readmission by center volume. Annual hospital case volume was calculated as the sum of all discharges with auto-HCT within the calendar year; low, medium, and high annual case volume groups were created based on (survey weighted) tertiles of patients (pts.) in the analytic data domain (Figure 1). Rates, causes, and costs of 30-day readmissions were compared between low-, medium-, and high-volume hospitals. The analysis was limited to urban teaching hospitals, and pts. admitted during month of December were excluded. The primary outcome was the unplanned 30-day re-admission following auto-HCT. Multiple logistic regression was used to model each 30-day readmission outcome including hospital case volume with other predictors (age, sex, disease type, primary insurance, median income, discharge disposition, co-morbidity, length of stay (LOS) and infection at index hospitalization).
Results: A total of 28,356 (weighted) auto-HCTs were performed during the time period and MM remains the most common indication (~60%). Baseline characteristics of pts. in low (<78/yr.)-, medium (78-187/yr.)- and high-volume (>187/yr.) hospitals were comparable as shown in Table 1. The overall rates of readmissions were significantly higher in low volume 15.7% (SE, 1.5) compared to medium 9.9% (1.5) and high volume 9.5% (1.8), p=0.002 centers. The mean time to readmission in low vs. medium vs. high volume centers was (8.3 [0.41] days vs. 10.7 [0.78] days vs. 8.9 [0.26] days; p <0.001); however, readmission LOS was significantly longer in low and medium volume centers (mean [SD], 7.2 [0.30] days vs. 8.3 [0.62] days vs. 6.2 [0.25] days; p=<0.001) respectively. Consequently, cost per readmission was significantly higher in low volume centers (mean [SD], $ 65,815 [3492] vs. $ 65,662 [5896] vs. $ 48,914 [4162]; p<0.001).
Readmission rates in low volume and medium volume centers compared to high volume centers were: adjusted odds ratio (aOR) 1.68, 95% CI 1.07-2.6; p =0.02 and 1.06 95% CI, 0.61-1.83; p=0.82, respectively. Other significant predictors of readmission included younger age (≥50 vs. <49) (aOR 0.81, 95% CI 0.68-0.98; p=0.03), female sex (aOR 1.20, 95% CI 1.06-1.36; p=0.003), disease type (others vs. MM) (aOR 1.37 95% CI 1.07-1.55; p= 0.018); and Elixhauser co-morbidity index (≥20 vs. 0; aOR 1.5, 95% CI 1.16-1.92; p= 0.00). Patients with non-routine discharges (discharges other than home) (aOR 1.3, 95% CI 1.1-1.7, p= 0.005), and shorter index LOS (aOR 0.94, 95% CI 0.89-0.98; p=0.01) were associated with higher readmission rates. The most common causes of readmission included: fever, neutropenia, infections, pneumonia, hyovolemia, nausea, vomiting and acute kidney injury.
Conclusions: This is the largest study till date reporting on the incidence and predictors of 30-day readmissions following auto-HCT in the US. The overall 30-day readmission rates following auto-HCT was ~12%. We report an inverse association with hospital auto-HCT volume (<78/yr.) and 30-day readmissions. Shorter LOS at index admission was associated with higher rates of readmission, which was associated with significantly higher cost to the health care system. These data should provide guidance when developing quality indicators and any policies penalizing hospitals for auto-HCT readmission.
Dhakal:Celgene: Consultancy, Honoraria; Takeda: Honoraria; Amgen: Honoraria. Shah:Lentigen Technology: Research Funding; Oncosec: Equity Ownership; Exelexis: Equity Ownership; Miltenyi: Other: Travel funding, Research Funding; Juno Pharmaceuticals: Honoraria; Geron: Equity Ownership. D'Souza:Takeda: Research Funding; Merck: Research Funding; Celgene: Research Funding; Prothena: Consultancy, Research Funding; Amgen: Research Funding. Hari:Spectrum: Consultancy, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Kite Pharma: Consultancy, Honoraria; Sanofi: Honoraria, Research Funding; Janssen: Honoraria; Amgen Inc.: Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding. Hamadani:Celgene Corporation: Consultancy; Ostuka: Research Funding; Cellerant: Consultancy; ADC Therapeutics: Research Funding; Janssen: Consultancy; MedImmune: Consultancy, Research Funding; Sanofi Genzyme: Research Funding, Speakers Bureau; Takeda: Research Funding; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal