Abstract
Introduction
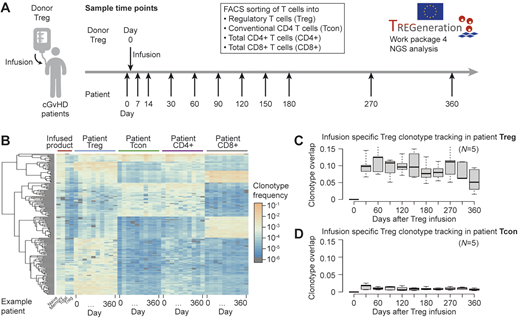
Under the auspices of the EC-Horizon 2020 project "TREGeneration", we are conducting five clinical phase I/II trials investigating the safety and efficacy of donor regulatory T cell (Treg) infusion in patients with chronic Graft-versus-Host Disease (cGvHD), a serious complication following hematopoietic stem cell transplantation (HSCT). Workpackage 4 evaluates T cell receptor (TCR) repertoire changes by high-throughput sequencing following the infusion of donor Tregs.
Methods
For repertoire analysis, four different T cell subsets (Treg, conventional CD4 T cells - Tcon, total CD4 and CD8 T cells) are FACS sorted from the infused product and from the cGvHD patients' peripheral blood before the infusion and at 10 time-points up to 12 months post infusion (Fig. 1A). To monitor TCR repertoire changes over time, we developed a novel quantitative "DeepImmune" technique for TCRβ amplification and sequencing. We amplify all TCRβ chain family transcripts from total RNA using a normalized primer set including molecular identifiers for unbiased and quantitative determination of TCRβ copy numbers. We have normalized the concentrations of our TCRβ primers using synthetic TCRβ gene sequences, thus minimizing amplification biases during RT-PCR to ≤3-fold differences among gene families. The inclusion of molecular identifiers during the RT-PCR step allows us to computationally remove additional biases introduced during the secondary PCR step for Illumina library preparation. Thus, our method results in ultra-deep characterization of immune receptor repertoires for sensitive detection of differences among samples and sample cohorts. Depending on T cell numbers in the samples, we routinely identify 1,000 - 150,000 clonotypes per sample.
Results
As first quality control for repertoire analysis, we cluster the top 200 TCRβ clonotypes from the different sequenced T cell subsets for each patient, resulting in heatmaps showing prominent repertoire differences among the analyzed T cell subsets (Fig. 1B; infused patient example shown). Next, we track the fate of infused donor Treg cells in the time course samples of the patients after Treg infusion, allowing us to quantify the number and frequency of TCRβ clonotypes that persist or expand in the patients after the infusion. We report that TCRβ clonotypes specific to the infused Treg cells (which were not present in the patients before Treg infusion) can be detected in the patients' blood after the infusion. Infusion-specific Treg clonotypes can reach up to 10-15% of the Treg repertoire of the patients and usually decline over time (Fig. 1C; boxplot shows clonotype overlap between infusion-specific Treg clonotypes and patient Treg clonotypes from five patients of the Lisbon cohort over 12 months). In the Tcon compartment of the patients, infusion-specific Treg clonotypes typically reach only 1-2% of the Tcon repertoire of the patients and also decline over time (Fig. 1D), similarly to what is observed in the CD8 T cell compartment (data not shown). This suggests that infused Tregs are not reverting to Tcons, an important control and promising result. We apply the same type of analysis to track clonotypes that were shared between the infused product and the patient prior to infusion, in addition to those clonotypes that were unique to the patient before infusion and not present in the infused product.
Conclusion
By applying our robust and sensitive TCRβ sequencing platform to samples from cGvHD patients infused with donor Treg, we are able to detect unique clonotypes of the infused product up to 1 year post-infusion. It remains to be be determined if there is any correlation between the level of detection of the infused clonotypes and the clinical responses of cGVHD to donor Treg therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal