Introduction
Infertility is a major late effect after allogeneic hematopoietic stem cell transplantation (HSCT). Post-transplant complications such as graft versus host disease (GVHD) may also impact health-related quality of life. The aim of this study was to evaluate sequalae of disease and transplant on fertility, pregnancy wish, affective and sexual life in female recipients.
Patients and methods
This unicentric prospective study was conducted from 2014 to 2016 in Saint Louis Hospital (Paris, France). To be included, women had to be a) aged > 18 years with a minimal follow-up of 2 years after an allogeneic HSCT b) younger than 35 at HSCT c) in persistent complete remission of their hematological disease. In the first part of the study, data related to affective, sexual life and pregnancies were collected by self-reported surveys. Responses to open-ended questions were analyzed using a thematic analysis approach. The second part, restricted to patients younger than 40 years at inclusion, evaluated post-transplant ovarian function by hormonal dosages. The study was approved by an institutional review board.
Premature ovarian failure (POF) was defined by amenorrhea and follicle stimulating hormone >25 IU/L.
Sixty-three patients were included at a median age of 31.3 years [IQR, 24.9-37.3]: 58 completed the survey and 34 were evaluated for ovarian function. Only 8 patients had already had children before HSCT. Median age at HSCT was 23.4 years [IQR, 18.3-28]. Twenty-nine (46%) patients were transplanted for acute leukemia and 16 (25%) for aplastic anemia. Conditioning regimen was myeloablative (MAC) in 39 patients (62%), reduced (RIC) in 22 (35%) and sequential in 2 (3%). Seventeen patients (27%) benefited from a fertility preservation procedure (82% performed after 2004): ovarian tissue cryopreservation alone (n=7) or associated with oocyte cryopreservation (n=9) (missing data n=1). Thirty-two (51%) patients experienced chronic GVHD and 16 (44% of assessed patients) gynecologic GVHD.
Results
Fifty patients (86%) reported hypoestrogenism symptoms, mainly vaginal dryness (n=44, 76%) and hot flushes (n=32, 55%). Forty-four patients (76%) reported negative impact of transplant on their sexual life: 18 (31%) a decrease in libido, 17 (29%) experienced dyspareunia, 14 (24%) highlighted a relationship between physical sequelae and sexuality, and 19 (33%) reported a loss of self-confidence. Twenty-seven patients (47%) indicated that disease and treatments had decreased their desire for pregnancy, mainly for fear of relapse, disease transmission, and also due to negative self-representation.
Most patients (n=56, 97%) were treated with hormone replacement therapy (HRT). Thirty-six patients (64%) temporarily interrupted their HRT. During this break, 14 (39%) experienced return of menses. POF was diagnosed in 25 of the 34 (74%) patients evaluated: 19/20 (95%) after MAC, 6/12 (50%) after RIC and none after sequential.
Twenty-two patients (38%) expressed a desire for pregnancy after transplant; among them, 9 (41%) had a child. In the whole population, 13 patients (21%) got pregnant: 8 naturally (1 after MAC and 7 after RIC or sequential regimen) and 5 through assisted reproductive technology. Natural pregnancy occurred in 2.6% (1/39) of patients after MAC, 22.7% (5/22) after RIC and 100% (2/2) after sequential conditioning regimen. Four of these 8 patients were transplanted for aplastic anemia, 2 for acute leukemia, 1 for sickle cell disease and 1 for lymphoma. Among patients who benefited from assisted reproductive technology, 4 resorted to oocytes donation and one had classical in vitro fertilization. Finally, 3 women adopted children.
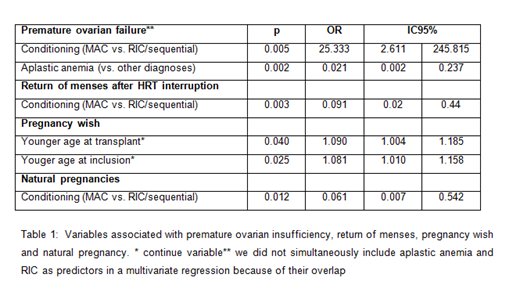
A univariate logistic regression analysis was performed to evaluate the impact of age at transplant and at inclusion, conditioning regimen, disease and chronic GVHD on post-transplant outcomes. Table 1 shows variables significantly associated with POF, return of menses, pregnancy desire and natural pregnancies.
Conclusion
This study highlights the major physical and psychological impact of disease and transplant on affective, sexual, and reproductive outcomes in women. In this series, RIC and sequential regimens allowed for post-transplant ovarian function preservation in more than 50% of patients. Improvement of post-transplant fertility and management of treatment impact on sexual and affective life has to be a priority in long-term survivors of HSCT.
Peffault de Latour:Amgen: Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Alexion: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding. Robin:Novartis Neovii: Research Funding. Michonneau:Neovii: Consultancy. Boissel:NOVARTIS: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal