Background: Minority patient (pt) populations are underrepresented in clinical trials and the proportion of such pts accrued to cancer studies has decreased, specifically among African Americans (AA) (Kwiatkowski et al. Cancer 2013). If minority pt populations have higher rates of comorbidities, restrictive eligibility criteria may contribute to systematic exclusion from studies. To explore the validity of this potential bias within AML pts, we characterized the comorbidity profile and compared outcomes between AA and white pts with AML.
Methods: Adult (≥18 years) AML pts who received chemotherapy at Cleveland Clinic from 2003 to 2019 were included. The following characteristics were analyzed: age, sex, self-reported race, insurance, etiology of AML, comorbidities, hepatic/renal function tests, left ventricular ejection fraction (LVEF), and corrected QT interval (QTc). AML risk was categorized according to the 2017 European LeukemiaNet (ELN) risk stratification. Organ dysfunction was defined as ≥ grade 1 per the Common Terminology for Adverse Events. Fisher's exact and Welch's t-tests were performed to compare baseline characteristics. Multivariable logistic and Cox regression analyses were used to identify prognostic factors for response status per International Working Group criteria, and overall survival (OS). Kaplan-Meier method and log-rank test were used to estimate and evaluate OS, respectively.
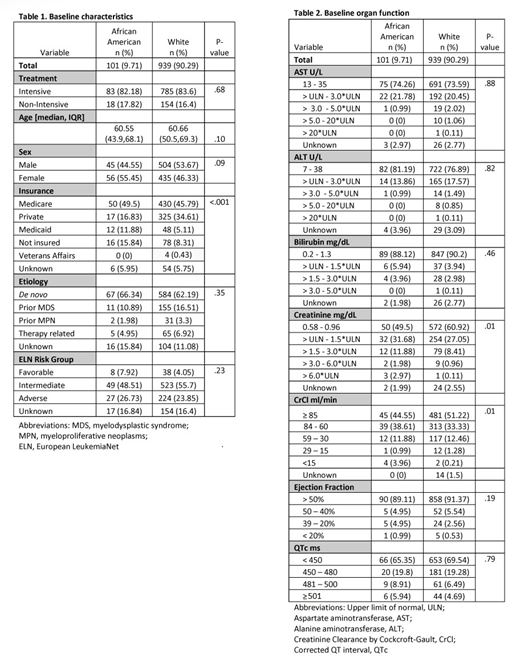
Results: Of 1,040 AML pts included, 939 (90.3%) identified as white and 101 (9.7%) as AA. Age, AML etiology, and AML risk were balanced between the two groups. Insurance coverage was different by race: AAs were more likely than whites to have Medicaid (11.9% vs. 5.1%), and less likely to have private insurance (16.8% vs. 34.6%), P<.001. Pts were treated with the following: 868 (83.5%) with intensive, cytarabine-based, and 172 (16.5%) with non-intensive (low-dose cytarabine or hypomethylating agents) regimens. AA pts were just as likely as whites to receive intensive therapy (P=.68) (Table 1).
AA pts presented with similar frequencies of both overall and specific comorbidities. Liver function laboratory values (AST/ALT/bilirubin) and cardiac test results (QTc/LVEF) at baseline were also similar; however, a greater proportion of AAs presented with renal dysfunction when compared to whites, as measured by creatinine (48.5% vs. 36.5%, P=.01) or creatinine clearance by Cockcroft-Gault (CrCl; 55.4% vs. 47.3%, P=.01; Table 2).
With a median follow-up of 12.73 months (IQR: 4.59-43.05), the OS for the cohort was 14.75 months (range: 0.03-189.25). Median OS did not differ by race (AA vs. whites: 13.7 vs. 14.9 months, P=.89). Overall, the complete response (CR) rate was 44.2%, which also did not differ by race: (AA vs. whites: 37.6% vs. 44.9%, P=.19). When adjusting for other known predictors, in a multivariable analysis, there was no difference in OS between AAs and whites (HR=1.20, P=.16); additionally, there was no association between comorbidities/organ dysfunction and OS, with the exception of liver comorbidities (HR=2.03, P=.002) and bilirubin (>1.5 x ULN vs. normal: HR= 1.69, P=.01). Clinically insignificant creatinine (>ULN - 1.5 x ULN vs. normal: HR= 0.99, P=.97) and CrCl (84-60 ml/min vs. normal: HR=0.96, P=.69) abnormalities were not independently associated with OS. Subgroup analyses by race revealed similar results for AAs, although, there were no differences in OS based upon bilirubin.
With the exception of liver comorbidities (OR= 0.17, P=.01), our analysis failed to identify significant evidence of association between response and comorbidities/organ dysfunction (similar results within the AA subgroup). Although AA were less likely to achieve a CR (AA vs. whites: OR=0.56, P=.05), there was no association between response and creatinine/CrCl abnormalities, regardless of severity.
Conclusions: Within this cohort, renal function eligibility criteria may be an important barrier to enrollment, specifically within the AA population. Since there is no association between clinically insignificant renal laboratory values and OS or response, the liberalization of such criterion may be justified. Future trials that broaden the renal function eligibility criterion have the potential to accrue more diverse pt populations, which may reduce recruitment racial disparities and improve the generalizability of the trials' results.
Hobbs:Amgen: Research Funding; SimulStat Inc.: Consultancy. Mukherjee:Bristol-Myers Squibb: Speakers Bureau; Takeda: Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Projects in Knowledge: Honoraria; Celgene Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Partnership for Health Analytic Research, LLC (PHAR, LLC): Consultancy; McGraw Hill Hematology Oncology Board Review: Other: Editor. Advani:Glycomimetics: Consultancy, Research Funding; Kite Pharmaceuticals: Consultancy; Amgen: Research Funding; Pfizer: Honoraria, Research Funding; Macrogenics: Research Funding; Abbvie: Research Funding. Gerds:CTI Biopharma: Consultancy, Research Funding; Pfizer: Consultancy; Incyte: Consultancy, Research Funding; Roche: Research Funding; Celgene Corporation: Consultancy, Research Funding; Sierra Oncology: Research Funding; Imago Biosciences: Research Funding. Nazha:Daiichi Sankyo: Consultancy; Incyte: Speakers Bureau; Jazz Pharmacutical: Research Funding; Abbvie: Consultancy; Tolero, Karyopharma: Honoraria; Novartis: Speakers Bureau; MEI: Other: Data monitoring Committee. Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Syros: Membership on an entity's Board of Directors or advisory committees; Millenium: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal