Introduction: Allogeneic hematopoietic stem cell transplantation (allo-HCT) provides a potential cure for a multitude of diseases but can result in high rates of morbidity and mortality. These outcomes have been associated with donor choice, with umbilical cord blood (UCB) perceived as an inferior option to matched related or matched unrelated donors (MRD/MUD) due to increased morbidity and mortality the first year after allo-HCT due to delayed engraftment and increased graft versus host disease (GvHD). At the same time, studies have shown that recipients of cells from younger donors do better, and UCB is the youngest donor cell source available. Given that UCB may have long-term benefits, we evaluated long-term survival in recipients of UCB vs. MRD/MUD in patients who had survived at least 1 year.
Methods: This is a retrospective analysis of ≥1 year (≥365 days) survivors of first allo-HCT from the Duke Adult Bone Marrow Transplant (ABMT) program over a twenty year period from January 1, 1996 to December 31, 2015. Detailed clinical data was extracted from the Duke ABMT database and electronic medical record. Patients who either died or were lost to follow-up within 1 year of transplant were excluded. Also excluded were those who received an allo-HCT for a disease other than a hematologic malignancy and those who received haploidentical or mismatched adult cells, as these donor sources have been associated with worse outcomes and the goal was to compare UCB to MRD/MUD. Patient characteristics included gender, race, ethnicity, transplant diagnosis, transplant year, hematopoietic cell transplantation-specific comorbidity index (HCT-CI), Karnofsky performance score (KPS) at transplant workup, age at transplant, donor cell characteristics, conditioning regimen, acute GvHD (aGvHD), date of relapse, and date of death. Chi-square tests or Fisher's exact tests were used to compare categorical variables, as appropriate, and Wilcoxon Rank Sum tests or t-tests were used to compare continuous variables, as appropriate. A Kaplan-Meier estimator was used to analyze overall survival. A Cox Proportional Hazard model with stepwise selection with significance of entry=0.1 and significance of stay=0.2 was used to evaluate the patient characteristics of age, gender, race, disease, KPS, conditioning type, history of aGvHD, and decade of transplant and adjusted for selected covariates to compare the two groups.
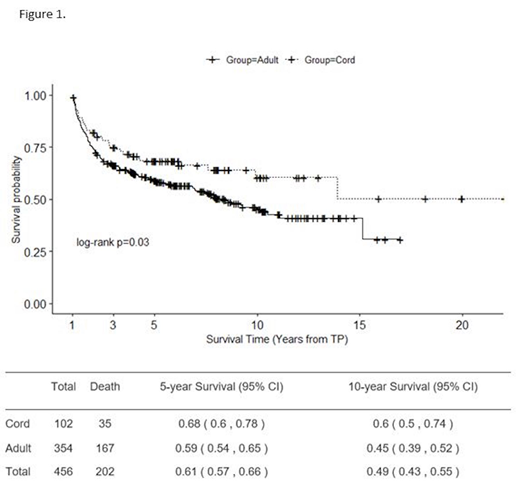
Results: Over the 20-year study period, 848 patients received a first allo-HCT, of whom 456 (54%) survived at least 1 year post-HCT: 102 (22%) UCB and 354 (78%) MRD/MUD. UCB recipients were more likely to be younger (median 42 years vs. 50 years, p=<0.001), African American (25% vs 6%, p<0.001), and have acute leukemia (70% vs. 49%, p=0.001). There were no differences in conditioning regimen (myeloablative conditioning 61% vs. 51%, p=0.08), pre-HCT performance status (KPS 80-100 87% vs. 82%, p=0.08), or comorbidities (HCT-CI ≤3 61% vs. 74%, p=0.052). With regard to post-HCT outcomes, UCB recipients had a higher rate of any aGvHD (70% and 59%, p=<0.001). Conditional on ≥1 year survival of allo-HCT, UCB recipients had a better unadjusted overall survival than adult cell recipients (Figure 1, log rank p=0.03). After adjusting for selected covariates (age, gender, conditioning type, decade of transplant), the hazard rate of UCB recipients was 37% lower than that of MRD/MUD recipients after the 1 year threshold, though this was no longer statistically significant (p=0.09).
Discussion: Among patients who survived at least 1 year post-HCT, those who received UCB had a significantly lower risk of mortality on univariate analysis than those who received adult cells. Though this finding was no longer statistically significant on multivariate analysis, there was a strong trend and the lack of statistical significance could be an effect of the small sample size. Additional research across larger populations (e.g. CIBMTR) is warranted to further explore the clinical characteristics and long-term health outcomes between the two groups, especially given the potential for newer UCB approaches such as ex-vivo expansion to decrease the early post-HCT morbidity and mortality associated with UCB and delayed engraftment. If other studies support improved long-term outcomes with UCB, those findings coupled with advances in UCB transplants may promote UCB as a donor source.
Gasparetto:Janssen: Consultancy, Honoraria, Other: Travel, accommodations, or other expenses paid or reimbursed ; BMS: Consultancy, Honoraria, Other: Travel, accommodations, or other expenses paid or reimbursed ; Celgene: Consultancy, Honoraria, Other: Travel, accommodations, or other expenses paid or reimbursed . Rizzieri:Celgene, Gilead, Seattle Genetics, Stemline: Other: Speaker; AbbVie, Agios, AROG, Bayer, Celgene, Gilead, Jazz, Novartis, Pfizer, Sanofi, Seattle Genetics, Stemline, Teva: Other: Advisory Board; AROG, Bayer, Celgene, Celltron, Mustang, Pfizer, Seattle Genetics, Stemline: Consultancy; Stemline: Research Funding. Horwitz:Abbvie Inc: Membership on an entity's Board of Directors or advisory committees. Sung:Novartis: Research Funding; Merck: Research Funding; Seres: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal