Introduction
Primary immune thrombocytopenia (ITP) is an autoimmune disease characterized by isolated thrombocytopenia. The pathogenesis of ITP mainly included immune-mediated platelet destruction and megakaryocyte maturation disorder. The first line therapy is steroid, but about one-third of patients do not respond to steroid. Recent studies have shown abnormalities in megakaryocyte growth and development and poorly compensated thrombopoiesis. It may be presumed that patients with these abnormalities may respond poorly to steroid and may be a candidate for therapy with thrombopoietin (TPO). The morphological classification of megakaryocytes in bone marrow may reflect the development of megakaryocytes, and may be associated with the response to steroid. Here, we intended to find out whether megakaryocytic morphology could be used to differentiate steroid-sensitive patients from primary ITP.
Methods
We retrospectively analyzed 170 patients with primary ITP who presented to the First Affiliated Hospital, Zhejiang University between May 2015 and Dec 2018. The diagnosis was made according to the International Working Group classification. Cases with secondary diseases that may cause thrombocytopenia were excluded. All patients were initially started on prednisolone 2 mg/kg. Response to steroid was defined as rise in platelet count to 50*109/L in 14 days. The patients who did not respond to steroid were given TPO along with the continuing dose of steroid. According to efficacy, patients were classified into 2 groups: steroid-sensitive and non-steroid-sensitive.
Bone marrow aspiration was performed at the time of diagnosis. The total number of megakaryocytes on whole slide was calculated by low-power microscope, and the morphology of as many as 50 megakaryocytes was analyzed by oil lens and classified to naïve, granular, thromocytogenic and naked nucleus megakaryocytes.
The correlation between the patients' clinical parameters and steroid-sensitive ITP was assessed using univariate logistic regression analyses. ROC curve analysis was performed to determine optimal cut-off values. We categorized these variables according to the cutoff values, and included these categorized variables for further multivariate logistic regression analyses. Then we constructed the predictive index on the basis of the independent factors included in the final multivariable logistic model.
Results
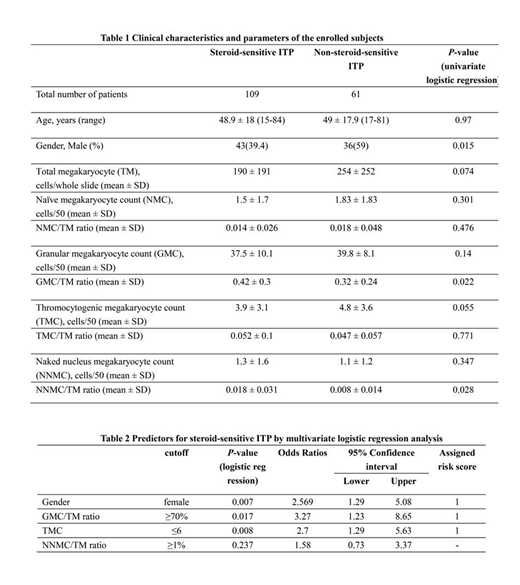
The clinical parameters of the included patients are shown in Table 1. A total of 109 and 61 patients were diagnosed as steroid-sensitive ITP and non-steroid-sensitive ITP. In univariate logistic model, the variables significantly associated with steroid-sensitive ITP were gender, thromocytogenic megakaryocyte count (TMC), the ratio of granular megakaryocyte count to total megakaryocyte count (GMC/TM ratio), and the ratio of naked nucleus megakaryocyte count to total megakaryocyte count (NNMC/TM ratio). Among the variables, female, reduced TMC with a cut-off value of 7, increased GMC/TM ratio with a cutoff value of 70% and elevated NNMC/TM ratio with a cutoff value of 1% showed diagnostic values with AUC values more than 0.5 in predicting steroid-sensitive ITP.
Multivariate logistic regression was used for the four significant variables identified by univariate analysis. According to the cut-off values, patients were classified into two categories. Gender (female; OR=2.569, 95%CI 1.29-5.08; P=0.007), reduced TMC (≤6; OR=2.7, 95%CI 1.29-5.63; P=0.008) and increased GMC/TM ratio (≥70%; OR=3.27, 95%CI 1.23-8.65; P=0.017) were found to be significantly independent predictors of steroid sensitivity (Table 2). On the basis of the regression coefficient and odds ratios, weighted risk scores of 1 were assigned to gender, TMC and GMC/TM ratio, respectively. The index resulted in total risk scores between 0 and 3. ROC analysis showed that an index greater than or equal to 2 points had the best AUC value (0.63) with 47.7% of sensitivity and 78.7% of specificity for predicting steroid sensitivity.
The non-steroid-sensitive ITP were subsequently treated with TPO, and 73% (30/41) responded to treatment.
Conclusions
The results showed that megakaryocytic morphology could be a good predictive marker for steroid-sensitivity. Steroid-sensitive ITP could be identified when primary ITP patients have a predictive index ≥ 2 points. These findings may help guide early treatment strategy in ITP.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal