Introduction
Choosing Wisely (CW) recommendations in Canada and the United States advise against routine blood work on stable inpatients because it is unlikely to improve patient care, is associated with anemia and pain, and increases costs. While numerous local quality improvement initiatives have effectively reduced the use of routine blood work (RBW), no population-level analyses have assessed the use of RBW on hospitalized patients in the CW era. This study aimed to describe the use of RBW between 2010 and 2017 by physicians caring for General Internal Medicine (GIM) inpatients at 7 hospitals. We hypothesized that RBW use would decrease over time and that increased use of RBW would be associated with greater reductions in hemoglobin.
Methods
We performed a retrospective cohort study using the General Medicine Inpatient Initiative (GEMINI) database, based in Ontario, Canada. The GEMINI database contains clinical and administrative data for all patients admitted to a GIM service at seven hospitals (5 academic centres; 2 community hospitals) in Toronto and Mississauga. We included all patients included in the GEMINI database, admitted from April 1, 2010 (prior to CW Canada), to March 31, 2017 (3 years after CW Canada's launch). Patients were excluded if they were admitted with a bleeding diagnosis, underwent an endoscopic or surgical procedure, were admitted to an Intensive Care Unit, or were admitted to hospital for less than 72 hours or greater than 30 days. Patients that received a blood transfusion during the first 48 hours of admission, or did not have hemoglobin measured within their first 48 hours of admission were also excluded. Physicians were excluded if they were the most responsible physician (MRP) for fewer than 100 admissions.
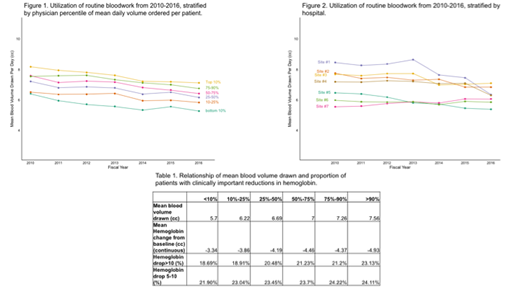
Our primary outcome was the mean volume of RBW ordered per patient per day by the MRP. RBW was defined as complete blood count, electrolytes, extended electrolytes, creatinine, liver panel, INR, or PTT. To examine changes in the distribution of RBW ordering over time, we report RBW use at the following physician percentiles: 10, 25, 50, 75, 90. Prior analyses of the relationship between RBW use and reduction in Hgb in hospital are confounded (sicker patients receive more bloodwork). To avoid this confounding, we examined change in Hgb among patients of physicians stratified by RBW use. Patients are quasirandomly allocated to physicians in GIM, and thus, observed differences can be attributed to physician practice, not patient factors. We report the mean change in Hgb as a continuous outcome, and also percentage of patients who experienced a clinically significant reduction in Hgb, which was prespecified as at least 10 g/L. Statistical significance was determined using Chi-square tests for categorical variables, and Kruskall-Wallis tests for continuous variables.
Results
We included 65,507 hospital admissions. The mean volume of RBW ordered per patient per day significantly decreased from 2010 to 2016, for all percentiles (p<0.001 for all percentiles; as an example: 7.23cc in 2010 to 6.17cc in 2016 for patients admitted to physicians in the 25-50th percentile) (Figure 1). The mean volume of RBW ordered per patient per day significantly decreased from 2010 to 2016 in all but one hospital (Figure 2). However, the spread between the 10th and 90th percentile physicians did not change much between 2010 (1.77cc/patient/day) and 2016 (1.84 cc/patient/day). There was a dose-response relationship between MRP use of RBW and reductions in patient Hgb (Table 1). Compared to patients of MRPs in the lowest 10% of RBW use, patients of physicians in the highest 10% had a greater mean reduction in Hgb (4.93 g/L vs 3.34 g/L, p<0.001), and were more likely to have a clinically significant reduction in Hgb (23.1% vs. 18.7%, p<0.001).
Conclusion
This large, multi-centre cohort study demonstrated that greater use of RBW on GIM inpatients was associated with clinically significant reductions in Hgb. To our knowledge, this is the first study to rigorously demonstrate that greater use of RBW may be associated with clinically meaningful reductions in Hgb, independent of patient-level confounding. We further found that RBW use decreased overall with time, and in 6 out of 7 hospitals, between 2010 and 2017. However, the spread between 10th and 90th percentile physicians has not changed, suggesting that opportunities still exist to reduce RBW use at both the hospital and physician level.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal