Introduction:
The majority of patients with Multiple Myeloma (MM) are elderly (≥ 65 years). High dose chemotherapy followed by autologous stem cell transplantation (HDCT-ASCT) is the standard of care in patients younger than 65 years. This treatment option should be individualized in elderly patients, mainly due to increased toxicity.
Goals:
To assess the safety and outcome of HDCT-ASCT in real life in patients ≥ 65 years of age with a diagnosis of MM.
Material and methods:
Retrospective cohort study of consecutive patients with a diagnosis of MM according to the IMWG 2014 criteria from a single academic center in Argentina, undergoing their first HDTC-ASCT during the period 2008- 2018. Patients with plasma cell leukemia or light chain amyloidosis were excluded. Data was extracted from medical records and collected in an standardized case report form. Consolidation treatment and maintenance were used according to the standard of institutional care at the time of the ASCT. The patients ≥ 65 years old at HDCT-ASCT were compared with those below < 65 years treated in the same period. Response were categorized as: complete remission (CR), very good partial remission plus partial remission (VGPR/PR) and stable disease plus progression disease (EE/PD). Overall response rate (ORR) included CR, VGPR and PR.
Overall survival (OS) and progression free survival (PFS) were calculated using the Kaplan and Meier method and compared using log-rank test. For survival, the risk ratio (HR) was calculated according to the multivariate Cox regression model. Transplant-related mortality (TRM) was analyzed with cumulative incidence curves of competitive risks. Values of p <0.05 were considered statistically significant.
Results:
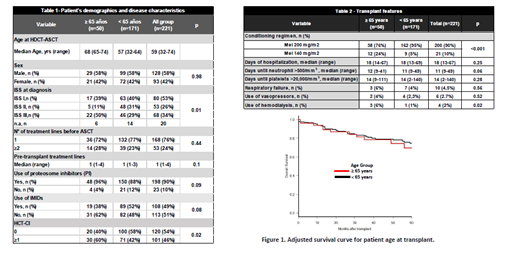
A total of 221 patients were included in the analysis: 50 patients ≥65 years (7 out of 50 > 70 years) and 171 patients <65 years. Patient's demographics and disease characteristics by age group are summarized in Table 1.
Reduced conditioning regimen (melphalan 140 mg/m2) was used in 5% of younger patients and 24% of older patients, p <0.001.
In the safety analysis, no significant differences were found between the two groups in the median days of hospitalization, duration of days of neutropenia or thrombocytopenia and life support measures during the period of hospitalization for the transplant (Table 2).
The TRM was 2.7% at 100 days (95% CI 1.1-5.5); there was no difference between patients ≥ 65 years and <65 years (2% vs. 2.9%, respectively; p = 0.928).
CR before transplant was 22% and 24% and at day 100 after ASCT 44% and 37% in patients ≥65 years and <65 years, respectively. For VGPR, corresponding rate were 64% and 67% before transplant and 79% and 77% at day 100 after ASCT in patients ≥65 years and <65 years, respectively. ASCT increased CR rate in both groups (p=0.050 and p=0.024, respectively).
After a median follow-up of 42.5 months (IQR 21-71.5), 3-year PFS was 56.2% (95% CI 39.8-70%) in ≥65 years and 58.2% (95% CI 49.6-65.9) in <65 years; (p = 0.86). The OS at 3 years was 78.3% (95% CI 62.1-88, 2) in ≥65 years and 79.3% (95% CI 71.6-85.1) in <65 years; (p = 0.94).
In the multivariate analysis including age at transplant, the quality of pre-transplant response (HR 0.08 for CR, p <0.001; HR 0.16 for VGPR/PR, p = 0.003) and the use of IP (HR 0.51; p = 0.047) were associated with better OS; while the age at transplant had no impact (HR 1.06; p=0.865) (Figure 1). For PFS , including age at transplant, only the quality of pre-transplant response demonstrated statistical significance (HR 0.06 for CR, p <0.001; HR 0.14 for VGPR/PR, p <0.001). Additionally, post-transplant maintenance, was independently associated with better OS (HR 0.34; p=0.016) and PFS (HR 0.47; p <0.001).
Conclusions:
Our data shows that it is feasible and safe to perform HDCT-ASCT in fit patients with multiple myeloma older than 65 years, and even in patients >70 years old. Patient selection should be based on frailty and comorbidities rather than chronological age alone. This group of patients experiences survival benefits similar to young patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal