Introduction: Large B-cell lymphoma (LBCL) is the most common subtype of non-Hodgkin lymphoma. Frontline treatment is curative in ~60% of patients (pts); however, ~30% of pts relapse and ~10% are refractory to frontline treatment. Treatment options for pts with relapsed/refractory (R/R) disease, especially in the third-line or greater (3L+) setting, have been primarily salvage chemotherapies (CTs). Recently, 2 CAR T cell products, axicabtagene ciloleucel (Yescarta®) and tisagenlecleucel (Kymriah®), and the antibody-drug conjugate, polatuzumab vedotin (Polivy®), were approved in the 3L setting. A systematic literature review (SLR) of R/R LBCL was conducted to identify relevant evidence on clinical outcomes in LBCL pts, including these new therapies, within the second-line and greater (2L+) or 3L+ setting, and to define the unmet medical need.
Methods: This SLR was conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and European Union Health Technology Assessment requirements. The review identified randomized and nonrandomized/observational studies within R/R LBCL, including diffuse large B-cell lymphoma (DLBCL), follicular lymphoma grade 3B (FL3B), primary mediastinal large B-cell lymphoma (PMBCL), DLBCL transformed from indolent lymphomas, and R/R DLBCL with secondary central nervous system (SCNS) involvement. Sources were EMBASE, MEDLINE, The Cochrane Library, and clinical conferences (ASCO, ESMO, EHA, ASH, ICML, AACR, and EORTC) from Jan 2000 to Apr 2019.
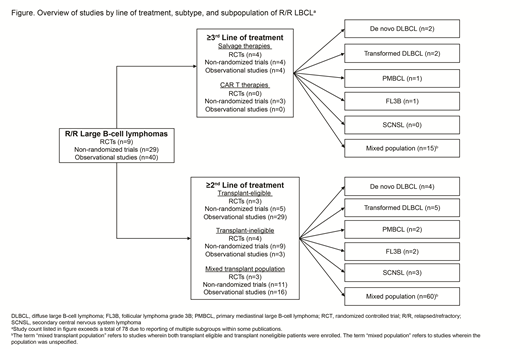
Results: Following screening of 8683 database records and additional sources, 103 publications covering 78 unique studies were identified. Studies identified were characterized by line of treatment and R/R LBCL subtype (Figure). OS, PFS, DOR, OR, and safety observed from the identified studies were described. Disease subtypes, pt eligibility criteria, and length of follow-up varied notably across studies.
In the 3L+ population, 11 salvage CT and 2 CAR T cell therapy studies reported survival outcomes. With salvage CT, the reported ORR across studies ranged from 0% to 54%, while CR ranged from 5.6%-31%. Median OS (mOS) ranged between 3-9 months, with one outlying study reporting mOS at 20 months. Median PFS (mPFS) reported within the salvage CT studies ranged from 2-6 months. Among CAR T cell therapies, pts treated with axicabtagene ciloleucel (n=101) reported a CR rate of 58% and median DOR (mDOR) was 11.1 months after a median follow-up of 27.1 months. mPFS was 5.9 months and mOS was not reached. At a median follow-up of 19.3 months, pts treated with tisagenlecleucel (n=115) had a CR of 40% but the mDOR was not reached. mOS was 11.1 months for all infused patients.
In the 2L+ transplant-eligible population (36 studies), pts who received high-dose CT + HSCT achieved mOS between 9 months to 5 years. In the transplant noneligible population, 16 studies reported mOS between 3-20 months. Studies involving mixed transplant-eligible and noneligible populations (30 studies) reported mOS of 1-17 months.
A few studies with limited sample sizes were found to report outcomes in LBCL subtypes (eg, PMBCL, SCNS lymphoma, DLBCL transformed from non-FL indolent lymphoma, FL3B). In the 3L+ setting, 1 study reported that mOS was not reached after a median of 6.6 months. In the 2L+ setting, 4 studies reported mPFS and mOS outcomes ranging between 2-9 months and 10-16 months, respectively.
Among studies assessing safety of salvage CTs in R/R LBCL, neutropenia, leukocytopenia, thrombocytopenia, and infections were the most commonly reported adverse events (AEs), with neutropenia being the most reported. Among the 3 studies reporting safety outcomes of CAR T cell therapy, data suggest that hematologic AEs (possibly related to lymphodepleting CT), cytokine release syndrome, and neurotoxicity are the most reported.
Conclusions: Despite the availability of new therapies for 2L+ and 3L + LBCL, examination of the current evidence has shown that there exists a high unmet need for additional therapeutic options that provide favorable benefit/risk and durable response for these patients. Furthermore, limited data are available for the rarer subtypes of LBCL. Both findings represent important treatment gaps for R/R LBCL that must be addressed in future research geared toward improvement of the current treatment landscape.
Maloney:Juno Therapeutics: Honoraria, Patents & Royalties: patients pending , Research Funding; Celgene,Kite Pharma: Honoraria, Research Funding; BioLine RX, Gilead,Genentech,Novartis: Honoraria; A2 Biotherapeutics: Honoraria, Other: Stock options . Liu:Celgene Corporation: Employment. Nientker:Celgene Corporation: Consultancy; Pharmerit Cöoperatief U.A.: Employment. Alleman:Pharmerit Cöoperatief U.A.: Employment; Celgene Corporation: Consultancy. Garcia:Celgene: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal