Introduction
Autoimmune hemolytic anemia is idiopathic in around half of the patients. However, it is known to be linked in the rest with autoimmune disorders, viral infections, drugs or cancers. The most common associated hematological malignancies are lymphoproliferative disorders, especially chronic lymphocytic leukemia (CLL).
The combination of CML and AIHA, on the contrary to CLL, is extremely unusual. In this review, we are going to shed the light on what is known so far about this association, patients' characteristics, how AIHA was treated and to analyze the possible underlying etiology .
Results
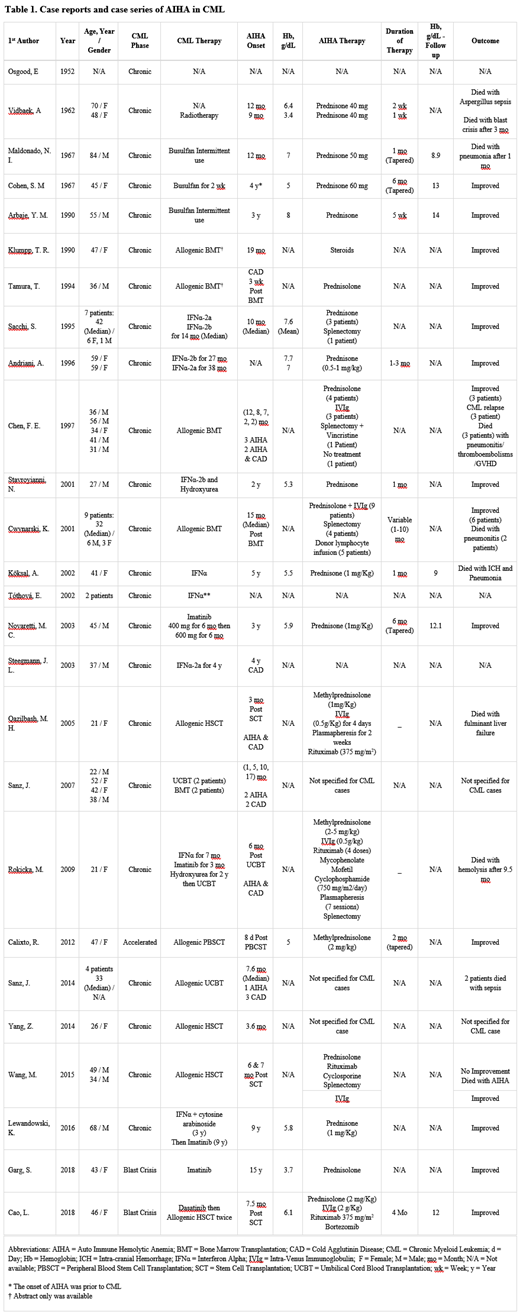
54 CML patients developed AIHA between 1952 and 2018 and summarized in Table 1. All of them were in the chronic phase of CML except 3 patients: one was in accelerated phase and two were in blast crisis. Different lines of therapy were used for CML: Among the 54 patients, one was treated with focused radiotherapy to the spleen, 3 were treated with Busulfan, 14 with IFNα, 4 were managed with Imatinib and 31 underwent allogenic hematopoietic stem cell transplantation (HSCT).
Warm AIHA was confirmed in 40 patients whereas cold agglutinin disease was confirmed in 7 patients and both types were diagnosed in 4 patients. The onset of AIHA was variable with median of 19 months after CML diagnosis in the non-transplant group. The onset of AIHA in the transplant group was earlier with median of 6.5 months. The median of Hemoglobin level at the time of diagnosis of AIHA was 5.9 g/dL (The lowest reported value was 3.4 g/dL and the highest reading was 8 g/dL).
It was noteworthy that almost half of the transplant patients had developed viral infections prior to the diagnosis of AIHA (12 due to CMV, 2 due to VZV, 1 due to Parvovirus and 1 due to Influenza virus). From the bone marrow transplanted group, 9 out of 18 cases were diagnosed with AIHA simultaneously with CML relapse.
AIHA was treated in 35 cases with Steroids. However, some required second- and third-line treatment with splenectomy (N = 8), IVIg (N = 16), Rituximab (N = 4), Bortezomib (N = 1) and Plasmapheresis (N = 2). More than half of all cases showed improvement with treatment. 14 patients passed away due to different reasons.
Discussion
The incidence of AIHA in patients with CML is extremely low, but when occurs, it almost always develops after the diagnosis of CML in the chronic phase. The rare occurrence and the variable onset of AIHA in those patients makes it difficult to claim that CML per say is the main culprit. In terms of the possible underlying etiology, patients might be classified into two categories: The hematopoietic stem cell transplant (HSCT) group, which constitutes more than half of the reported cases in this review, and the non-transplant group, which was treated with Busulfan, Interferon or Imatinib.
Hemolysis post HCST is rare but well-known complication and is categorized into either alloimmune or autoimmune. The etiology of AIHA in HSCT group is thought to be related either to the donor cell immune reconstitution, concomitant viral infection, or CML relapse.
The cause of AIHA in the non-transplant group is thought to be linked to drugs used specifically for CML treatment, despite that the mechanism behind it is poorly understood. Interferon was more frequently reported than both Busulfan and Imatinib combined. It was suggested that hemolysis, in case interferon was used, is mediated either by the formation of immune complexes or through the possible modification of red blood cell surface antigens and production of autoantibodies. New onset severe anemia due to Imatinib is very unusual. It was hypothesized that the mechanism behind it is either because of imatinib effect on hematopoietic stem cells or through an interaction with iron absorption or metabolism, despite that iron replacement didn't improve the outcome.
In terms of prognosis, many patients responded well to steroids as first line, but physician should keep in mind that second- and third-line treatment might be required in transplanted patients. Clinician should be aware that despite AIHA is uncommon in CML patients, it should be in the differential diagnosis list for those who develop a sudden drop of hemoglobin without source of bleeding.
Conclusion
AIHA is a rare cause of anemia in CMl , but when occurs, it develops after the diagnosis of CML in the chronic phase which usually respond to steroids . AIHA that develop in CML patients after transplantation usually required more than steroid therapy to control it.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal