TO THE EDITOR:
The presence of measurable residual disease (MRD) in patients with acute myeloid leukemia (AML) is an important prognostic factor in all stages of the disease.1-5 In particular, patients in a morphologic remission who still have detectable MRD prior to allogeneic transplant have an outcome similar to patients with morphologically persistent disease pretransplant, at least when conventional polymerase chain reaction (PCR)- and flow cytometry–based techniques are used to identify MRD. However, the molecular heterogeneity of AML has rendered it challenging to develop any assay that can consistently detect residual disease, and most methods available today lack sensitivity beyond 1 cell in 100.
In the randomized trial of chemotherapy plus or minus the FLT3 inhibitor midostaurin for FLT3-mutant AML (CALGB10603/RATIFY), patients who underwent allogeneic transplant in remission after treatment with chemotherapy plus midostaurin had a markedly better outcome posttransplant compared with patients on the control arm who were transplanted after achieving remission with chemotherapy alone.6 The assumption has been that patients on the midostaurin arm had a lower level of MRD, although the means to determine this have thus far not been available. We have developed a highly sensitive combination PCR–next-generation sequencing (NGS) MRD assay for FLT–internal tandem duplication (ITD) mutations and validated this assay using paired diagnosis and remission samples from FLT3-ITD AML patients. Our results offer clear support for the aforementioned assumptions regarding the RATIFY trial.
The assay is depicted in supplemental Figure 1A, available on the Blood Web site. PCR (10 cycles) was performed using primers flanking exons 13 and 15 to amplify the FLT3 gene. Highly diverse NGS libraries were generated using additional PCR cycles and sequenced using Illumina’s sequencing-by-synthesis method. Using a custom bioinformatics approach, unique FLT3-ITD mutations of varying lengths were identified, and mutant allelic frequencies were calculated. DNA from FLT3-ITD mutant clinical samples and cell lines (MV4-11, PL-21, and MOLM-13) was either tested neat or after being spiked into DNA derived from healthy blood donors to evaluate the assay’s sensitivity and linearity (supplemental Figure 1B).
We validated the assay using clinical samples from a series of 17 patients with FLT3-ITD AML (clinical features summarized in Table 1). All 17 patients had an FLT3-ITD mutation, a canonical C-terminal frameshift NPM1 mutation, and an intermediate risk karyotype. All patients received a single course of infusional cytarabine and anthracycline–based (eg, intensive) chemotherapy, and all achieved a complete remission conforming to international working group criteria.7 In all 17 samples, multiparameter flow cytometry detected no leukemia by immunophenotype in the remission samples. Although 7 patients received time-sequential induction therapy (AcIVP16; Table 1), previous studies have shown a comparable remission rate between 7 + 3 and time-sequential therapy for FLT3-ITD-mutated AML.8,9 The capillary electrophoresis (CE) PCR assay to detect FLT3-ITD mutations was negative in the remission sample for all 17 cases. In each case, this was after a single course of treatment, and the remission biopsy was performed a mean of 40 days (range 29 to -58 days) after the start of induction. Unfortunately, because these were banked DNA samples, an RNA-based quantitative PCR assay for NPM1 mutations could not be performed. All 17 patients underwent allogeneic transplant in first remission, and all had diagnostic and remission DNA samples banked in accordance with an institutional review board–approved protocol conforming to the Declaration of Helsinki. One specific criterion that we did not select for, but realized only in retrospect, was that 9 of these patients received chemotherapy alone, whereas 8 received chemotherapy plus an FLT3 tyrosine kinase inhibitor (gilteritinib-4; midostaurin-3; sorafenib-1). The investigators performing the MRD assay were blinded to the clinical data.
Patient characteristics and FLT3-ITD results
| Patient number . | Age/sex . | Induction therapy . | ITD mutation by CE-PCR at diagnosis . | ITD mutation by MRD assay at diagnosis . | ITD mutation by MRD assay at remission . | Clinical outcome . | |||
|---|---|---|---|---|---|---|---|---|---|
| Length, bp . | VAF, % . | Length, bp . | VAF . | Length, bp . | VAF . | ||||
| 1 | 59/F | AcIVP16 | 51 | 5 | 51 | 7.7 | 51 | 0.0017 | Alive, disease free 5 y after diagnosis |
| 30 | 30 | 1.42 | 30 (ND) | 0 | |||||
| 2 | 56/F | AcIVP16 | 51 | 37 | 51 | 47.48 | 51 | 0.0027 | Alive, disease free 5 y after diagnosis |
| 3 | 64/M | AcIVP16 | 81 | 46 | 81 | 75.69 | 81 | 0.020 | Alive, disease free 3 y after diagnosis |
| 4 | 67/M | 7 + 3 + gilteritinib | 21 | 5 | 21 | 3.93, 0.16 | None detected | 0 | Alive, disease free 1 y after diagnosis |
| 60 | 0 | ||||||||
| 5 | 67/F | AcIVP16 | 18 | 9 | 18 | 11.09 | 18 | 0.0077 | Alive, disease free 4 y after diagnosis |
| 30 | 0.10 | 30 (ND) | 0 | ||||||
| 39 | 0.35 | 39 (ND) | 0 | ||||||
| 6 | 56/M | 7 + 3 + gilteritinib | 51 | 81 | 51 | 85.77 | 51 | 0.06 | Alive, disease free 2.5 y after diagnosis |
| 7 | 52/M | AcIVP16 | 27 | 5 | 24 | 0.57 | 24 | 0.2 | Relapsed with the 42-bp ITD, died of relapsed disease 2 y after diagnosis |
| 42 | <5 | 27 | 5.68 | 27 | 0.099 | ||||
| 93 | <5 | 42 | 0.75 | 42 | 0.1 | ||||
| 96 | <5 | 63 | 0.20 | 63 | 0.22 | ||||
| 93 | 7.02 | 93 (ND) | 0 | ||||||
| 96 | 11.45 | 96 | 0.013 | ||||||
| 8 | 31/F | 7 + 3 + midostaurin | 15 | 45 | 15 | 45.27 | 15 | 0.004 | Alive, disease free 2 y after diagnosis |
| 9 | 72/F | 7 + 3 + midostaurin | 33 | 5 | 33 | 6.48, 0.32 | 33 | 0.005 | Alive, disease free 2 y after diagnosis |
| 69 | 69 (ND) | 0 | |||||||
| 10 | 68/F | 7 + 3 | 24 | 37 | 24 | 39.53 | 24 | 0.018 | Alive, disease free 4 y after diagnosis |
| 11 | 57/F | AcIVP16 | 15 | 45 | 15 | 44.39 | 15 | 0.04 | Relapsed with the 15-bp ITD and died 1 y after diagnosis |
| 12 | 43/M | 7 + 3 + midostaurin | 60 | 30 | 60 | 38.36 | 60 | 0.008 | Alive, disease free 2 y after diagnosis |
| 13 | 67/F | 7 + 3 + gilteritinib | 27 | 10 | 27 | 25.52, 1.87 | 27 | 0.003 | On gilteritinib maintenance after transplant, relapsed with AML lacking ITD |
| 108 | 108 (ND) | 0 | |||||||
| 14 | 47/M | 7 + 3 + sorafenib | 72 | 4 | 72 | 30.97 | 72 | 0.005 | Died of GVHD 19 mo after diagnosis |
| 15 | 68/F | 7 + 3 | 45 | 31 | 45 | 46.7 | 45 | 2.17 | Alive, disease free 4 y after diagnosis |
| 16 | 60/M | 7 + 3 + gilteritinib | 24 | 36 | 24 | 37.63 | 24 | 0.004 | Alive, disease free 2 y after diagnosis |
| 17 | 44/F | AcIVP16 | 48 | 72 | 48 | 70.37 | 48 | 0.031 | Alive, disease free 5 y after diagnosis |
| Patient number . | Age/sex . | Induction therapy . | ITD mutation by CE-PCR at diagnosis . | ITD mutation by MRD assay at diagnosis . | ITD mutation by MRD assay at remission . | Clinical outcome . | |||
|---|---|---|---|---|---|---|---|---|---|
| Length, bp . | VAF, % . | Length, bp . | VAF . | Length, bp . | VAF . | ||||
| 1 | 59/F | AcIVP16 | 51 | 5 | 51 | 7.7 | 51 | 0.0017 | Alive, disease free 5 y after diagnosis |
| 30 | 30 | 1.42 | 30 (ND) | 0 | |||||
| 2 | 56/F | AcIVP16 | 51 | 37 | 51 | 47.48 | 51 | 0.0027 | Alive, disease free 5 y after diagnosis |
| 3 | 64/M | AcIVP16 | 81 | 46 | 81 | 75.69 | 81 | 0.020 | Alive, disease free 3 y after diagnosis |
| 4 | 67/M | 7 + 3 + gilteritinib | 21 | 5 | 21 | 3.93, 0.16 | None detected | 0 | Alive, disease free 1 y after diagnosis |
| 60 | 0 | ||||||||
| 5 | 67/F | AcIVP16 | 18 | 9 | 18 | 11.09 | 18 | 0.0077 | Alive, disease free 4 y after diagnosis |
| 30 | 0.10 | 30 (ND) | 0 | ||||||
| 39 | 0.35 | 39 (ND) | 0 | ||||||
| 6 | 56/M | 7 + 3 + gilteritinib | 51 | 81 | 51 | 85.77 | 51 | 0.06 | Alive, disease free 2.5 y after diagnosis |
| 7 | 52/M | AcIVP16 | 27 | 5 | 24 | 0.57 | 24 | 0.2 | Relapsed with the 42-bp ITD, died of relapsed disease 2 y after diagnosis |
| 42 | <5 | 27 | 5.68 | 27 | 0.099 | ||||
| 93 | <5 | 42 | 0.75 | 42 | 0.1 | ||||
| 96 | <5 | 63 | 0.20 | 63 | 0.22 | ||||
| 93 | 7.02 | 93 (ND) | 0 | ||||||
| 96 | 11.45 | 96 | 0.013 | ||||||
| 8 | 31/F | 7 + 3 + midostaurin | 15 | 45 | 15 | 45.27 | 15 | 0.004 | Alive, disease free 2 y after diagnosis |
| 9 | 72/F | 7 + 3 + midostaurin | 33 | 5 | 33 | 6.48, 0.32 | 33 | 0.005 | Alive, disease free 2 y after diagnosis |
| 69 | 69 (ND) | 0 | |||||||
| 10 | 68/F | 7 + 3 | 24 | 37 | 24 | 39.53 | 24 | 0.018 | Alive, disease free 4 y after diagnosis |
| 11 | 57/F | AcIVP16 | 15 | 45 | 15 | 44.39 | 15 | 0.04 | Relapsed with the 15-bp ITD and died 1 y after diagnosis |
| 12 | 43/M | 7 + 3 + midostaurin | 60 | 30 | 60 | 38.36 | 60 | 0.008 | Alive, disease free 2 y after diagnosis |
| 13 | 67/F | 7 + 3 + gilteritinib | 27 | 10 | 27 | 25.52, 1.87 | 27 | 0.003 | On gilteritinib maintenance after transplant, relapsed with AML lacking ITD |
| 108 | 108 (ND) | 0 | |||||||
| 14 | 47/M | 7 + 3 + sorafenib | 72 | 4 | 72 | 30.97 | 72 | 0.005 | Died of GVHD 19 mo after diagnosis |
| 15 | 68/F | 7 + 3 | 45 | 31 | 45 | 46.7 | 45 | 2.17 | Alive, disease free 4 y after diagnosis |
| 16 | 60/M | 7 + 3 + gilteritinib | 24 | 36 | 24 | 37.63 | 24 | 0.004 | Alive, disease free 2 y after diagnosis |
| 17 | 44/F | AcIVP16 | 48 | 72 | 48 | 70.37 | 48 | 0.031 | Alive, disease free 5 y after diagnosis |
All 17 patients had normal/intermediate karyotype and NPM1 mutation at diagnosis. All 17 patients achieved complete remission after a single cycle of induction therapy, and all underwent allogeneic transplant in first remission. Chemotherapy regimens: AcIVP16 = Cytarabine 2000 mg/m2 continuous infusion days 1 to 3, idarubicin 8 mg/m2 per day on days 1 to 3, etoposide 400 mg/m2 per day on days 8 to 10; 7 + 3 = cytarabine 100 to 200 mg/m2 per day on days 1 to 7, idarubicin 12 mg/m2 per day on days 1 to 3.
GVHD, graft-versus-host disease; ND, not detectable; VAF, variant allele frequency.
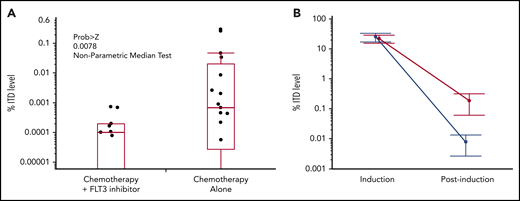
The MRD assay results were compared with the conventional CE PCR assay results for diagnostic and remission time points. At diagnosis, the MRD assay detected 100% of the ITD mutations detected by the CE assay, and in 6 of the 17 cases, it detected additional (1 to 6) ITD mutations (Table 1). In the remission samples, the MRD assay detected persistence of the diagnostic ITD mutation in 16 out of 17 cases. Although the %ITD levels between diagnosis and remission were statistically significant in all patients (Figure 1; P value 6.315e-06 to 7.78e-05 using Wilcoxon rank sum test), more striking was the fact that in the 8 patients treated with chemotherapy plus an FLT3 inhibitor during induction, the average level of ITD mutation was significantly lower compared with the 9 patients treated with chemotherapy alone (see Figure 1 for %ITD level values; P = .0078 by the nonparametric median test). In addition to the median test, a Wilcoxon rank sum test corroborated the statistical significance between these groups (P = .04563). The 1 patient (Table 1 patient 4) who had no detectable ITD mutation in the remission sample had received 7 + 3 (cytarabine 100 mg/m2 per day for 7 days, idarubicin 12 mg/m2 per day for 3 days) plus 120 mg/d of gilteritinib from days 4 to 17 of induction. The time between the start of induction and remission/MRD assessment was similar between the 2 groups (inhibitor group: mean 40.5 days; no inhibitor group: mean 40 days). Although this data set is small, these findings are consistent with the concept that when FLT3 inhibition is combined with induction chemotherapy, the result is a deeper remission, which may translate into better posttransplant survival.
FLT3-ITD levels before and after induction. Banked genomic DNA samples from the patients listed in Table 1 were analyzed by MRD assay. (A) One-way analysis of the difference in FLT3-ITD levels at remission, comparing patients treated with chemotherapy only with patients treated with chemotherapy plus an FLT3 inhibitor. (B) Graphic comparison of an FLT3-ITD level decrease from diagnosis to remission. Although the difference in %ITD levels between induction and postinduction is statistically significant in both groups (P value 6.315e-06 for −FLT3, and P value 7.78e-05 for patients with chemotherapy plus FLT3 inhibitor using Wilcoxon rank sum test), the %ITD levels in patients with chemotherapy only are much higher than in the former group, and the difference between such groups at the postinduction level is significant (P value .04563 on a Wilcoxon rank sum test).
FLT3-ITD levels before and after induction. Banked genomic DNA samples from the patients listed in Table 1 were analyzed by MRD assay. (A) One-way analysis of the difference in FLT3-ITD levels at remission, comparing patients treated with chemotherapy only with patients treated with chemotherapy plus an FLT3 inhibitor. (B) Graphic comparison of an FLT3-ITD level decrease from diagnosis to remission. Although the difference in %ITD levels between induction and postinduction is statistically significant in both groups (P value 6.315e-06 for −FLT3, and P value 7.78e-05 for patients with chemotherapy plus FLT3 inhibitor using Wilcoxon rank sum test), the %ITD levels in patients with chemotherapy only are much higher than in the former group, and the difference between such groups at the postinduction level is significant (P value .04563 on a Wilcoxon rank sum test).
FLT3-ITD mutated AML is a common variant of this leukemia with an obvious, trackable genetic lesion, an ITD within the juxtamembrane domain.10 Use of this mutation for monitoring MRD has a disadvantage in that it is not stable: it can occasionally be lost at relapse, or, alternatively, it is detected only at relapse.11,12 However, it has the advantage of specificity: each patient’s mutation tends to be unique in size (ranging from 3 to >200 bp in length) and insertion site. It therefore acts as a mutational signature of the patient’s AML, particularly because these mutations tend to be the final “hit” in leukemogenesis.13 Sensitive detection of FLT3-ITD mutations in remission bone marrow specimens using conventional PCR is hampered by template bias, in which the reaction enzymes preferentially amplify the shorter wild-type sequence.14,15 Conventional NGS approaches are generally designed to detect point mutations or short insertions/deletions and likewise lack sensitivity beyond what flow cytometry can routinely detect (eg, 0.1% to 1%). However, the novel combination assay that we describe here can detect a targetable mutation and potentially influence treatment decisions. Although we have presented evidence that the assay is very sensitive, its positive predictive value is undetermined. Furthermore, we focused on a chemo-responsive group of patients: those with a concomitant NPM1 mutation. The clinical impact of this assay might be different in patients harboring more adverse genotypes. Therefore, the next questions (answered, it is hoped, from ongoing randomized clinical trials) include whether this type of assay can identify patients at risk of relapse, and potentially to validate the utility of maintenance therapy with FLT3 inhibitors. In addition, more refined flow cytometry methods are in development that will no doubt complement this PCR-NGS approach.
This assay will be used to measure MRD levels in subjects enrolled on Quantum-First (#NCT02668653), a phase 3 trial of patients with FLT3-ITD AML randomized to receive chemotherapy plus the FLT3 inhibitor quizartinib or placebo. A similar assay is being used in BMT-CTN1506 (“Morpho”), a randomized trial of gilteritinib vs placebo as posttransplant maintenance therapy for FLT3-ITD AML.16
Further data are available by e-mailing the corresponding author.
Authorship
Contribution: M.L. designed the study, analyzed the data, and wrote the manuscript; C.G. and E.A. contributed samples and helped edit the manuscript; W.S., C.L., R.P., and J.L. developed the NGS assay, contributed to study design, analyzed data, and helped edit the manuscript; and K.C., F.B., and A.L. contributed to study design and helped edit the manuscript.
Conflict-of-interest disclosure: M.L. serves as a consultant for Daiichi-Sankyo, Novartis, Astellas, Amgen, Arog, and Agios. W.S., C.L., R.P., and J.L. are employees of Navigate BioPharma Services, Inc. K.C., F.B., and A.L. are employees of Daiichi-Sankyo. The remaining authors declare no competing financial interests.
Correspondence: Mark Levis, Kimmel Cancer Center at Johns Hopkins, 1650 Orleans St, Room 2M44, Baltimore, MD 21287; e-mail: levisma@jhmi.edu.
REFERENCES
Author notes
The online version of this article contains a data supplement.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal