Abstract
Introduction - Acute myeloid leukemia (AML) is an aggressive disease with a relapse rate of approximately 40% in children. Progress in improving cure rates has been slow, in part because AML is very heterogeneous. Molecular studies consistently show that most cases are comprised of distinct subclones that diminish or expand over the course of therapy. Single-cell profiling methods now allow parsing of the leukemic population into subsets based on gene and/or protein expression patterns. We hypothesized that comparing the features of the subsets that are dominant at relapse with those that are dominant at diagnosis would reveal mechanisms of treatment failure.
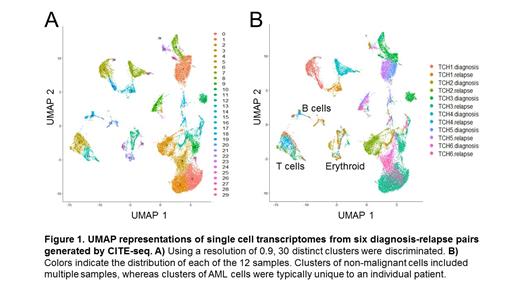
Methods - We profiled diagnosis-relapse pairs from 6 pediatric AML patients by Cellular Indexing of Transcriptomes and Epitopes by Sequencing (CITE-Seq). All patients were treated at Texas Children's Cancer Center and consented to banking of tissue for research. CITE-Seq was performed by Immunai (New York, NY) using a customized panel of 65 oligonucleotide-tagged antibodies, the 10x Genomics Chromium system for single-cell RNA library generation, and the Novaseq 6000 for sequencing. After data cleanup and normalization, clustering by scRNA-seq was done using the Seurat package. Cell-type identification of clusters was facilitated by published healthy bone marrow scRNA-seq datasets (van Galen et al, Cell 2019). Differentially expressed genes (DEGs) and proteins (DEPs) between diagnosis and relapse were determined using Wilcoxin ranked sum tests.
Results - We generated single-cell transcriptomes for a total of 28,486 cells from 12 samples, with a mean of 2373 cells and 1416 genes per sample. Samples were integrated with batch effect correction, producing 30 distinct clusters (cell types) in total (Figure 1A). Cell types with expression profiles consistent with lymphocytes and erythroid precursors were identified in multiple patients, whereas AML cell types tended to be specific to individual patients (Figure 1B). For patients TCH1, TCH2 and TCH3, the most abundant cell types at diagnosis were rare at relapse, and cell types that were rare at diagnosis became dominant at relapse. For these 3 cases, we identified DEGs between the dominant diagnosis cell types and dominant relapse cell types. We found 18 genes that were upregulated at relapse in at least 2 of the cases. Several genes related to actin polymerization were enriched (ARPC1B, ACTB, PFN1), possibly reflecting an enhanced capacity for adhesion and migration. Also of note, macrophage migration inhibitory factor (MIF) and its receptor CD74 were upregulated at relapse, suggesting a role in chemoresistance. For patients TCH4, TCH5 and TCH6, the same cell types that were abundant at diagnosis were also abundant at relapse, and few genes were significantly altered between diagnosis and relapse in multiple cases. Only SRGN, which encodes the proteoglycan serglycin, and GAPDH were altered in 2 of these 3 cases, and both were downregulated at relapse. We performed similar comparisons to identify proteins that were differentially expressed between diagnosis and relapse pairs. The number of DEPs between the dominant diagnosis and relapse cell types ranged from 0 (TCH1 and TCH6) to 5 (TCH2). The only protein altered in more than one case was CD7, which was enriched at relapse in TCH2, TCH3 and TCH4.
Conclusions - From CITE-Seq profiling of 6 pediatric AML cases we identified two distinct patterns of relapse. For 3 cases, relapse occurred by expansion of a subset that was small but present at diagnosis. Enrichment of genes associated with adhesion and survival signaling suggests that these cells survived because they were well-equipped to take advantage of interactions with the microenvironment. For 3 other cases, the population that was dominant at diagnosis persisted and expanded at relapse with few substantial changes in gene or protein expression profiles. This pattern suggests that these AML cells were a priori equipped to survive chemotherapy, even though bulk disease levels were transiently reduced below the limit of detection. Most profiled proteins did not change substantially between diagnosis and relapse. An exception is CD7, which was enriched at relapse in 50% of our cases and represents a potential therapeutic target. Analysis of more cases will refine these relapse patterns, reveal potential mechanisms of chemoresistance and inform the development of novel therapies.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal