Abstract

Introduction: VEXAS syndrome, caused by somatic mutations in ubiquitin-like modifier activating enzyme 1 (UBA1) gene, is a late-onset and progressive autoinflammatory disease. Main hematologic manifestations include macrocytic anemia, thrombocytopenia, and dyspoiesis. Concomitant diagnoses of myelodysplastic syndrome (MDS) and plasma cell dyscrasia (PCD) are common. Venous thromboembolism (VTE) and arterial thrombosis (AT) have been reported. We describe the incidence and characteristics of thrombosis in a large cohort of 86 patients with VEXAS syndrome, along with detailed coagulation profiles in a subgroup of patients. We also explore potential predictors of thrombosis, and effect on overall survival (OS).
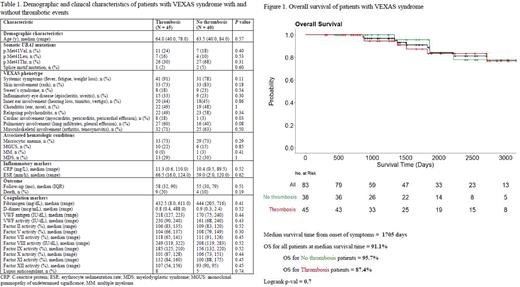
Methods: Two cohorts of patients with confirmed VEXAS were included. Thirty patients were evaluated at the National Institutes of Health (NIH) Clinical Center and 56 patient records reviewed from referring institutions. Logistic regression models were used to determine predictors of thrombosis. Cox proportional hazards models and Kaplan Meier curves were used for survival analysis.
Results: The total population consisted of 86 patients. Eighty-five patients (99%) were male with a median age of 64 years (range, 40-84 years) at disease onset. Hematologic manifestations included macrocytic anemia in 63 (73%), MDS in 25 (29%) and PCD in 17 (20%) patients.
Thrombosis occurred in 45 patients (52%); 41 (48%) had VTE and 11 (12%) had AT, with a median time to event from disease onset of 18 and 34 months, respectively; five patients (5%) had both VTE and AT. Among VTE, there were 26 (30%) deep venous thrombosis (DVT), 12 (14%) pulmonary embolism (PE), and 7 (8%) superficial thrombophlebitis. Twenty-two (54%) of VTE cases were unprovoked. Recurrent VTE was seen in 15 (17%) of patients, among which 9 (53%) occurred while receiving anticoagulation. Arterial events included myocardial infarction in 7 (8%) patients, stroke in 2 (2%) patients, and peripheral arterial occlusion in 2 (2%) patients. Recurrent AT was seen in 2 (2%) patients.
Patients from the NIH cohort underwent extensive coagulation testing. Fourteen patients (46%) had a positive lupus anticoagulant (LA), which was persistently positive 12 weeks apart in 8 of 9 patients re-tested. Of these 8 patients, 6 had a VTE, 1 had a stroke and 1 did not have thrombotic manifestations. Thirteen patients (43%) with thrombotic events were negative for LA. Median levels of fibrinogen, D-dimer, Factor (F) VII, FIX, and especially von Willebrand factor (VWF) and FVIII, were high in 15 tested VEXAS patients, but there was no significant difference between those with and without thrombosis (Table 1). Of 10 patients with high VWF and 17 with high FVIII activity, 6 (60%) and 9 (53%) had a thrombotic event, respectively; these correlated with high levels of CRP and ESR. No patients were found to have abnormal antithrombin III activity, Factor V Leiden, or prothrombin gene mutations.
No difference in age, UBA1 gene mutation, median levels of CRP and ESR, presence of MDS or PCD was found between patients with or without thrombosis; MDS, PCD and UBA1 gene mutation were also not predictive of thrombosis. Among inflammatory disease manifestations, cardiac involvement (myocarditis, pericarditis, or pericardial effusion) correlated with the presence of any thrombosis (p = 0.03). When considering VTE alone, cardiac manifestations strongly predicted PE and DVT (p = 0.004 and p = 0.005 respectively), while the presence of chondritis correlated with PE (p = 0.02). Presence of thrombosis did not impact OS (Figure 1).
Conclusions: Patients with VEXAS syndrome are at high risk of thrombosis, mainly venous, which can be recurrent despite anticoagulation therapy. The underlying etiology remains unclear, but many VEXAS patients have positive LA, high VWF and FVIII levels, suggesting inflammation, endothelial activation and/or an immune process as pathophysiologic. Cardiac manifestations, including myocarditis, pericarditis, and pericardial effusion, significantly correlated with thrombosis in general, while chondritis correlated with presence of PE. Presence of thrombosis did not impact OS. Given the high incidence of thrombosis, VEXAS patients should be carefully risk assessed for VTE and considered for prophylactic anticoagulation, and indefinite treatment if thrombosis has occurred.
Disclosures
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal